| Abstract |
Amoebiasis is a common intestinal protozoan infection due to Entamoeba histolytica. In India, the prevalence of the disease varies from 2% to 67%.[1] Acute Fulminant Colitis is a rare complication of intestinal amebiasis. Life threatening lower Gastrointestinal bleed is very rare presentation of amebiasis. Here, we are presenting a case of severe lower GI bleed proved to be caused by amebiasis along with extra intestinal complications.
Keywords: Colitis, Entamoeba histolytica, lower GI bleed
| How to cite this article: Dogra V K, Gupta D, Kashyap R, Nand L, Sondhi S. Intestinal amebiasis presenting as life threatening lower GI bleed-A rare presentation. Ann Trop Med Public Health 2017;10:244-6 |
| How to cite this URL: Dogra V K, Gupta D, Kashyap R, Nand L, Sondhi S. Intestinal amebiasis presenting as life threatening lower GI bleed-A rare presentation. Ann Trop Med Public Health [serial online] 2017 [cited 2017 Jul 15];10:244-6. Available from: https://www.atmph.org/text.asp?2017/10/1/244/205554 |
| Introdution |
Amoebiasis is a common intestinal protozoan infection due to Entamoeba histolytica with an annual mortality between 50,000 and 110,000 due to the various complications associated with the invasive disease. In India, the prevalence of the disease varies from 2% to 67%.[1] Amebiasis is the second leading cause of death from parasitic disease worldwide. Symptoms range from mild diarrhea to severe dysentery producing abdominal pain, diarrhea, and bloody stools (94-100%). Acute Fulminant colitis is a rare complication of intestinal amebiasis and tends to occur in approximately less than 1% of cases but it is associated with high mortality rate of more than 50%.[2] We are presenting a young patient admitted with lower GI bleed and was found to have acute fulminant colitis and liver abscess caused by E. histolytica.
| Case Report |
A 42-year male presented with history of fever since 10 days and bleeding per rectum since 2 days. Bleeding was severe and patient was in shock when presented to emergency department.
On physical examination patient’s PR was 108/min and blood pressure was 80/30 mmHg. Per rectal examination finger was soiled with blood, no faecal matter present. His Hb was 2.9 gm/dl, Total Leukocyte Count 33110/m.[3] Colonoscopy showed multiple bleeding colonic ulcers [Figure 1], on chest x-ray right side pleural effusion [Figure 2], on ultrasound and CT abdomen there was 17 × 14 × 14 cm abscess in right lobe of liver with rupture in right pleural cavity [Figure 3], amoebic serology was positive for E. histolytica and HIV ELISA was non reactive. Stool was negative for E. histolytica cysts and trophozoites. Colonic biopsy taken was negative for E. histolytica microscopy.
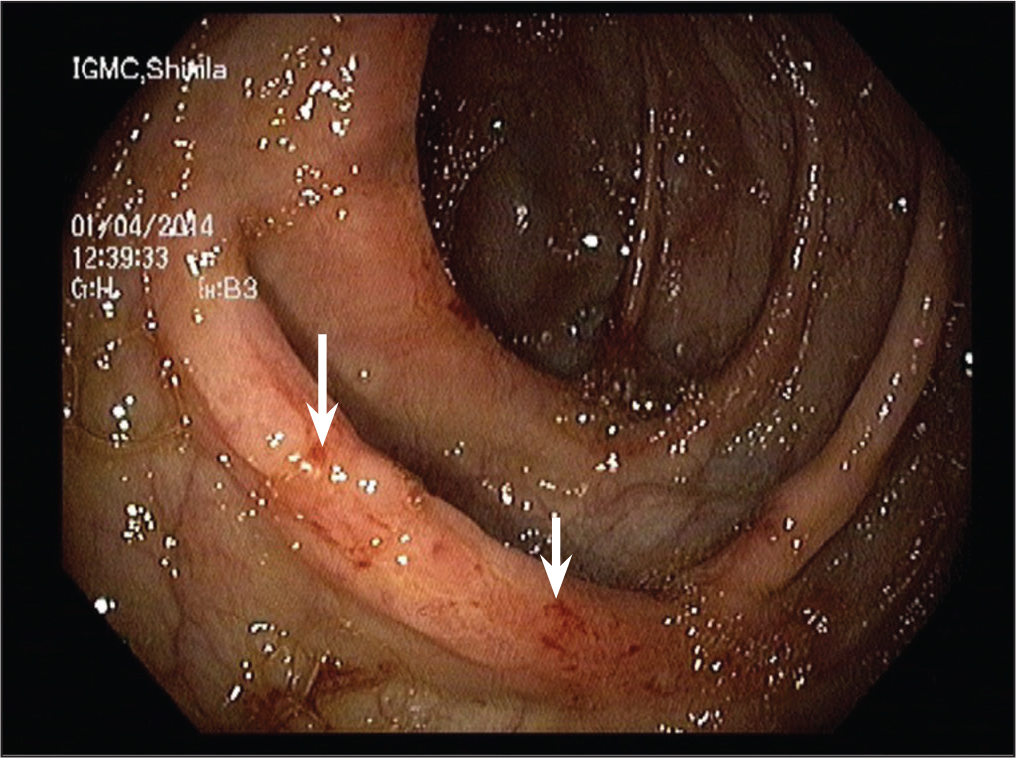 |
Figure 1: Multiple colonic ulcers
Click here to view |
| Figure 2: Chest x-ray right pleural effusion
Click here to view |
| Figure 3: CT abdomen showing right lobe liver abscess
Click here to view |
Course and management in hospital
Patient was managed with seven units of blood transfusions, injection metronidazole 750 mg three times a day, injection ceftriaxone 1 gm two times a day. Pig tail catheter aspiration of liver abscess done. Patient responded to treatment. His pleural effusion improved [Figure 3]. His pus was investigated for amoebiasis by microscopic examination but was negative.
In spite of absence of cyst and trophozoites in pus, stool, and biopsy of colon diagnosis of amoebic ulcers with amoebic liver abscess was kept due positive serology and response to metronidazole.
| Discussion |
Amoebiasis is a common intestinal protozoan infection due to E. histolytica with extra intestinal manifestations. Worldwide annual mortality is estimated to be 50,000-110,000 due to the various complications associated with the invasive disease.[3] Ninety percent of E. histolytica infection is asymptomatic, which usually spontaneously resolves within 12 months. Among those 10% with clinical amebiasis the onset is generally subacute for 1-3 weeks. Symptoms range from mild diarrhea to severe dysentery producing abdominal pain, diarrhea, and bloody stools (94-100%). Fever and weight loss are present in less than 40% of patients.[4],[5] Acute fulminant colitis is a rare complication of intestinal amebiasis and tends to occur in approximately less than 1% of cases but it is associated with high mortality rate of more than 50%.[4] Diagnosis of intestinal amebiasis depends mainly on histopathology and the presence of flask shaped ulcers in the mucosa. In our cases, the diagnosis was difficult to make from the clinical presentation or even colonoscopic findings. It was only possible to reach the final diagnosis by history of fever and lower GI bleed, on investigations pyothorax right side, colonic ulcers on colonoscopy, positive serology, and above all response to metronidazole. Stool microscopy is a relatively poor method because it has low sensitivity (30%).[5] In our cases, stool examination was negative for ameba. Antigen detection assays of the stool are one of the best current means, they are sensitive, specific, rapid, easy to perform; but the test is not currently available in our laboratory.[5] Serology with antibody measurements is widely available, with high sensitivity of 95% of amebic liver abscess, but the problem is that it may remain positive for years; which might give false positive result, especially in endemic area.[6] But in our patient clinical profile and response to therapy was favoring amebic etiology so the positive serology was taken as evidence of resent amebic infections. So in all patients coming with lower GI bleed infective causes as amebiasis should be ruled out especially in areas where amebiasis is endemic. For diagnosis antigen based tests which are underused, have got better sensitivity and specificity, ideally should be done before starting the treatment.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest
| References |
| 1. |
Sehgal R, Devi R. Secretory IgA as a marker of invasive amoebiasis. Rev Infect 2010;1:235-38.
|
| 2. |
Al-Saad S, Al Khwaja SA, Georage SM, Jundaid M, Moheb K. Fuulminant Amebic colitis a Life Threatening Rare Entity. Bahrain Med Buloetin. 2009:31. http://www.bahrainmedicalbulletin.com/ march 2009/amebic colotis.pdf.
|
| 3. |
Walsh JA. Problems in recognition and diagnosis of amoebiasis. Estimation of the global magnitude of morbidity and mortality. Rev Infect Dis 1986;8:228-38.
|
| 4. |
Aristizabal H, Acevedo J, Botero M. Fulminant amebic colitis. World J Surg 1991;15:216-21.
|
| 5. |
Petri WA. Recent advances in amebiasis. Crit Rev Clin Lab Sci 1996;33:1-37.
|
| 6. |
Patterson M, Healy GR, Shabot JM. Serologic testing for amebiasis. Gastroenterology 1980;78:136-41.
|
Source of Support: None, Conflict of Interest: None
| Check |
DOI: 10.4103/1755-6783.205554
| Figures |
[Figure 1], [Figure 2], [Figure 3]



