|
Ascaris lumbricoides is a common intestinal parasite in tropical and temperate regions. Although usually asymptomatic, infection can lead to biliary or intestinal obstruction and very rarely obstruction of the main pancreatic duct due to its smaller lumen. We report two cases of ascariasis in the main pancreatic duct, which is not a common site, presenting as acute pancreatitis and recovering uneventfully with conservative management.
Keywords: Ascariasis, Endoscopic Retrograde Cholangio Pancreatography, Hepato Pancreato-Biliary System, Pancreatitis
How to cite this article:
Darlong LM, Das R, Hajong R, Topno N. A report of two cases of ascariasis pancreatitis managed conservatively. Ann Trop Med Public Health 2011;4:48-50 |
How to cite this URL:
Darlong LM, Das R, Hajong R, Topno N. A report of two cases of ascariasis pancreatitis managed conservatively. Ann Trop Med Public Health [serial online] 2011 [cited 2016 Aug 19];4:48-50. Available from: https://www.atmph.org/text.asp?2011/4/1/48/80537 |
Ascaris lumbricoides infects more than a quarter of the total world population and is particularly common in Asia, Africa and Central America. [1] Poor socioeconomic condition and fecal contamination of soil around the dwelling causes infection in 30% of adult and 60-70% of children. Ascariasis infestation in intestine is usually asymptomatic. But it creates problems when it enters the hepato pancreato-biliary system when there is heavy duodenal infestation. However, invasion of the pancreatic duct is rare, presumably secondary to its smaller caliber [2] and a part of the worm usually remains in duodenum. The worm usually moves back into the duodenum in 24-48 hours after producing biliary or pancreatic symptoms or both.
Case 1
A 28-year-old female presented to us with acute abdominal pain of 1 day, colicky in nature, starting at the epigastric region and radiating to the back. Patient had nausea but no vomiting or fever. She had similar attack 2 years back, and was relieved with analgesics. On physical examination, the patient was afebrile, had a pulse rate of 96/min and blood pressure (BP) of 90/60 mmHg, with epigasric tenderness but no guarding or rigidity and normal bowel sounds. A complete blood count demonstrated normal leukocyte count of 6800/mm 3 , normal liver enzymes with elevated serum amylase (1724 IU/l) and serum lipase (8640 IU/l). Ultrasonogram of the abdomen revealed a round worm in main pancreatic duct with normal ductal caliber [Figure 1]. The pancreas was visualized throughout and it appeared bulky with a hazy outline but no peripancreatic collection. The gallbladder and common bile duct lumen was normal though round worms were seen in the small bowel. The patient was managed conservatively with bowel rest, intravenous fluids, analgesics-antispasmodics and proton pump blockers and was symptom free from the 2 nd day of admission. Follow-up ultrasonogram done 3 days after relief of symptom showed a normal pancreatic size, outline, parenchyma echogenicity and worm free main pancreatic duct. Patient was discharged on 10 th day of admission with albendazole. Follow-up ultrasonogram done after a month showed a normal biliopancreatic tree.
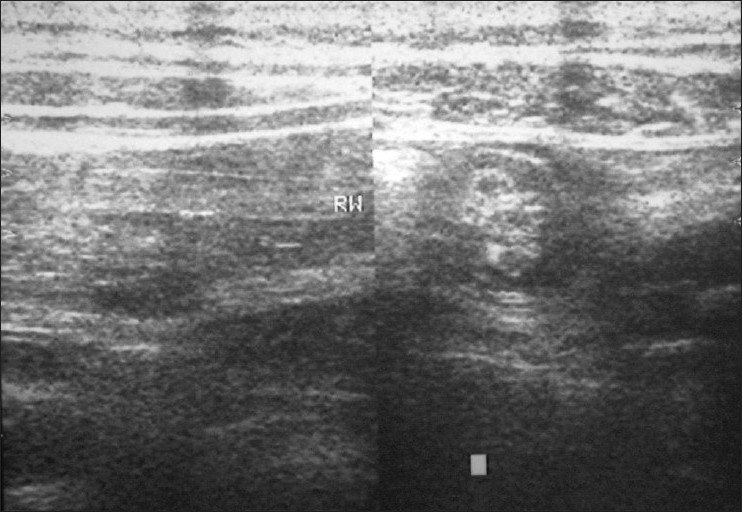 |
Figure 1: Long, linear echogenic strips without acoustic shadowing in the pancreatic ducts (the “strip” sign) which on transverse scan appears as target lesions.
Click here to view |
Case 2
A 30-year-old female was admitted with acute abdominal pain in the epigastrium and right hypochondrium along with episodes of vomiting, of 1 day duration. On physical examination, she was afebrile, with a pulse rate of 88/min and a BP of 110/70 mmHg, and with abdomen eliciting tenderness in the right hypochondrium and epigastrium with no guarding or rigidity and normal bowel sounds. A complete blood count demonstrated a leukocyte count of 10,000/mm 3 , normal liver enzymes and elevated serum amylase (2000 IU/l) and serum lipase (5670 IU/l). The ultrasonogram of the abdomen showed a round worm in the main pancreatic duct with a bulky pancreas and no peripancreatic collection. The patient was also managed conservatively with bowel rest, analgesics-antispasmodics, intravenous fluid, proton pump blocker and was symptom free from the 3 rd day of admission. Follow-up ultrasonogram done after 5 days showed a normal pancreas with no evidence of worm. Following this, the patient was discharged on the 9 th day of admission with albendazole.
A. lumbricoides is the most common helminthic infection in humans and occurs when Ascaris eggs are ingested from infected soil, food, or water. Larvae emerge in the duodenum and then migrate to the cecum, where they access veins of the portal system and are transported to the liver. From the hepatic veins, larvae pass to the heart and lungs . After migrating up the tracheo-bronchial tree, the larvae are swallowed and the mature worms develop in the small intestine over several months, and eggs are passed in the feces [1] to continue the life cycle. The worms move freely in and out of the hepato pancreato-biliary tree and therefore can be easily missed. Stool studies may show Ascaris ova and dead worm; parasite detection by stool examination for ova may approach 100%. [3] The diagnosis of pancreatic ascariasis can be done with ultrasonogram, endoscopy/endoscopic retrograde cholangio pancreatogram (ERCP), computed tomography (CT) or magnetic resonance cholangio pancreatogram (MRCP). Ultrasonography is a simple, noninvasive and highly accurate test reflecting the worm morphology which may be single or multiple, long, linear echogenic strips without acoustic shadowing in the biliary or pancreatic ducts (strip sign). [4] In transverse scanning, the hepato pancreato-biliary worms produce a bull’s eye appearance. This has a sensitivity of 50-86% for worms in the biliary tree, but the sensitivity for detecting worms in the pancreatic duct is not known. Endoscopic imaging can demonstrate active worms within the duodenal lumen and ampulla. At ERCP, Ascaris worms can be identified as smooth, linear filling defects within the ducts. [1] ERCP images may also show the worms as parallel smooth filling defects or as curves or loops traversing the ducts. [5] Use of ERCP allows better identification of worms in the duodenum and in the pancreatic-biliary tree, while providing a safe, therapeutic option of removing the worms. A CT scan can also be useful for diagnosis but has a lower sensitivity than ultrasonography. Though not routinely used, MRCP findings of pancreatic Ascaris have been best demonstrated on T2-weighted images as linear filling defects within a dilated pancreatic duct. [6]
With appropriate conservative management, worms spontaneously return to the duodenum in 98% of children and 94% of adults. [1] Parenteral antispasmodics to relax the sphincter, analgesics for pain, intravenous fluid and bowel rest are recommended during acute attacks. In these cases, endoscopic intervention is reserved for patients who (a) fail conservative therapy or (b) have worms in the ducts after 3 weeks of observation. [1],[7] Other authors advocate emergent endoscopy if hepato pancreato-biliary ascariasis is suspected, in an attempt to clear the pancreatic and biliary ducts of all roundworms and prevent serious complications. [8] Worm extraction by using a basket or forceps without sphincterotomy results in rapid relief of signs and symptoms and is successful in 90-98% of patients. [8] Anthelmintic therapy with mebendazole or albendazole started once the acute attack subsides is effective in eradicating ascariasis in 84-100% of cases. Despite the excellent results, patients can have a reinvasion from either reinfection or ineffective therapy, with a reported incidence of 15-28% at 1 year. In endemic areas, anthelmintic therapy must be repeated every 2 monthly. The prognosis of Ascaris-induced pancreatitis is excellent if the patient is diagnosed and treated early. The mortality rate is 3% in endemic areas. Follow-up after successful treatment of acute stage involves stool examination and ultrasonography. The above-mentioned two cases share same clinical features like short duration of abdominal pain, less physical signs but raised levels of amylase and lipase, with ultrasonogram being a reliable tool to diagnose and follow-up the cases and both cases resolving on conservative management. If ascariasis infection is suspected and subsequent investigations confirm the diagnosis, initial conservative management can be followed where ERCP facility is not available and the patient’s condition does not deteriorate. Most of the time, those live Ascaris come out from the hepato pancreato-biliary system and the symptoms subside spontaneously and anthelmintic drugs are started once the hepato pancreato-biliary system is free of worm.
| 1. |
Khuroo MS. Ascariasis. Gastroenterology Clin NorthAm 1996;25:553-77. |
| 2. |
Khuroo MS, Zargar SA, Yattoo GN, Koul P, Khan BA, Dar MY, et al. Ascaris-induced acute pancreatitis. Br J Surg 1992;79:1335-8. |
| 3. |
Khuroo MS, Zargar SA, Yattoo GN, Koul P, Khan BA, Dar MY, et al. Ascaris-induced acute pancreatitis. Br J Surg 1992;79:1335-8. |
| 4. |
Ferreyra NP, Cerri GG. Ascariasis of the alimentary tract, liver, pancreas and biliary system: Its diagnosis by ultrasonography. Hepatogastroenterology 1998;45:932-7. |
| 5. |
Bhushan B, Watal G, Mahajan R, Khuroo MS. Endoscopic retrograde cholangiopancreaticographic features of pancreaticobiliary ascariasis. Gastrointest Radiol 1988;13:327-30. |
| 6. |
Kenamond CA, Warshauer DM, Grimm IS. Ascaris pancreatitis. Radio Graphics 2006;26:1567-70. |
| 7. |
Khuroo MS, Zargar SA, Yattoo GN, Javid G, Dar MY, Boda MI, et al. Worm extraction and biliary drainage in hepatobiliary and pancreatic ascariasis. Gastrointest Endosc 1993;39:680-5. |
| 8. |
Sandouk F, Haffar S, Zada MM, Graham DY, Anand BS. Pancreatic-biliary ascariasis: Experience of 300 cases. Am J Gastroenterol 1997;92:2264-7. |
Source of Support: None, Conflict of Interest: None
DOI: 10.4103/1755-6783.80537
[Figure 1] |