| Abstract |
Objective: The aim of this study is to estimate the status of cutaneous manifestations in HIV-infected patients and its co-relationship with the CD4 cell count at a tertiary care centre at Bastar, Jagdalpur. Material and Methods: In this study, 137 HIV-positive subjects were enrolled. Information on demographics i.e. weight, height, socioeconomic status, age, educational status, sex, laboratory parameters (CD4 counts) and treatment regimens were noted, and patients were examined for skin disorders by a dermatologist. Data were analyzed using Chi-square test for categorical variables. Results: Majority of the patients resided in a rural area (65.69%), and belonged to low socioeconomic and educational status; 30.65% were housewives, 23.35% drivers and 16.78% laborers respectively. The predominant mode of transmission was heterosexual contact (94.16%). The most common HIV-related dermatological manifestations were seborrheic dermatitis (74.16%), xerosis (52.5%), generalized skin hyperpigmentation 56 (46.67%), onychomycosis 53 (44.16%), pruritic papular eruption 27 (22.5%), oral candidiasis 21 (17.5%), photo dermatitis 21 (17.5%) and scabies 4 (3.33%). Significant correlation with low CD4+ cell counts was found for oral candidiasis (P<0.0001) and Kaposi’s sarcoma (P 0.03), while other disorders like seborrheic dermatitis (P 0.22), xerosis (P 0.25) and onychomycosis (P 0.08) were not statistically significant. Conclusion: This study showed a high prevalence of dermatological manifestations in HIV-infected subjects, and they occur more frequently with progression of HIV and decline in immune functions. So, early diagnosis and management of skin disorders can improve the quality of life of HIV-infected subjects.
Keywords: Human immune deficiency, national aids control organization, people living with HIV/AIDS
| How to cite this article: Singh H, Singh P, Tiwari P, Dey V, Dulhani N, Singh A. HIV-infected patients and dermatological manifestations in a tertiary care hospital in the tribal (Bastar) region of Chhattisgarh, India between January 2006 and June 2008. Ann Trop Med Public Health 2010;3:64-7 |
| How to cite this URL: Singh H, Singh P, Tiwari P, Dey V, Dulhani N, Singh A. HIV-infected patients and dermatological manifestations in a tertiary care hospital in the tribal (Bastar) region of Chhattisgarh, India between January 2006 and June 2008. Ann Trop Med Public Health [serial online] 2010 [cited 2020 Aug 14];3:64-7. Available from: https://www.atmph.org/text.asp?2010/3/2/64/77188 |
| Introduction |
A total of 39.5 million (34.1 million-47.1 million estimated) people were living with HIV in 2006, [1] this includes the estimated 4.3 million (3.6 million- 0.6 million) adults and children who were newly infected with HIV in 2006. New, more accurate estimates indicate that approximately 2.5 million (2 million-3.1 million) people in India were living with HIV in 2006, and that adult national HIV prevalence was 0.36%. Although the proportion of people living with HIV is lower than previously estimated. [2] The highest number of PLHA is in Andhra Pradesh and Maharashtra. Manipur and Nagaland have the highest prevalence, due to small population size. According to NACO 2006, HIV prevalence in Chhattisgarh was 0.17%; it was maximum (1.67%) in Manipur and minimum (0.03%) in Himanchal Pradesh. [3] In Chhattisgarh, Durg district has maximum HIV burden and Bastar is the second highest. These are categorized as Category A and C respectively. [4] HIV infection constitutes a main health problem [5],[6],[7] worldwide. Dermatological disorders are a health problem among HIV-positive patients which present with a variety of manifestations. [8],[9] Among HIV-infected individuals, skin diseases cause significant morbidity and frequently may be initial signs of immunosuppression, [10] they affect between 80 and 95% of dermatological manifestations in HIV-infected patients according to the literature, [11],[12] occurring at any time in the course of infection. Skin is often the first and only organ affected during most of the course of the HIV disease. [11],[13],[14] Cutaneous disorders during HIV infection are numerous. [15],[16] Some cutaneous disorders reflect the progression of HIV disease, [13],[15] but this relation is still controversial. [16],[17] Extensive HIV-related literature has focused on distinctive clinical presentations such as Kaposi’s sarcoma, oral hairy leukoplakia and oral candidiasis. [15],[17] However, the findings on careful skin examination of HIV-infected patients who present for primary care have received limited attention. In this study we describe systematic dermatological manifestations of HIV-infected patients on initial presentation.
| Materials and Methods |
This is a prospective study which was conducted in Govt. Medical College and associated Maharani Hospital, Jagdalpur (C.G.) between January 2006 and June 2008. Patients were collected from OPD, in ward, and from counseling centre, all participants testing positive for HIV at screening for ongoing study. A total of 137 consecutive HIV-positive subjects were enrolled during this period. There were no specific eligibility criteria. All HIV-positive patients who accessed care at the hospital were included. Information on demographics, e.g., age, sex, height, weight, SES, educational status, laboratory parameters (CD4+ counts) and treatment regimens were noted [Table 1]. A complete medical history and physical examination of patients were done by a dermatologist for optimal evaluation and diagnosis of dermatologic lesions on the basis of clinical appearance. Data were analyzed, using the chi square test for establishing correlation between CD4+ cell counts and various dermatological disorders, P value < 0.05 was considered clinically significant.
| Table 1: Demographic parameters of HIV-infected patients
Click here to view |
| Results |
The results of this study showed that among 137 HIV patients, 83 (60.58%) were males and 54 (39.41%) were females. Of these, most patients (54, 39.41%) were in 30-39 years age group (19 females and 35 males), while female prevalence was highest (18.97%) in the age group of 20-29 years. Majority of the patients (90, i.e., 65.69%) were residing in rural areas. Of these sufferers, 79.56% belonged to the lower socioeconomic status; only 1.45% were from high socioeconomic class. Of our subjects, the largest group was housewives (30.65%), the second largest groups being drivers 32 (23.35%) and laborers 23 (16.78%) respectively. Majority of the patients had low education, 37 (27%) educated only up to the 5 th standard and 36 (26.27%) up to high school, while 22 (16.05%) were illiterate. One hundred and thirty-one (95.62%) subjects were Hindus, the rest were from other religions. The predominant mode of transmission was heterosexual contact (94.16%), only one patient (0.72%) was infected through transfusion of infected blood, seven (5.10%) patients acquired infection via vertical (mother to child) transmission [Table 2]. [There was no history of intravenous drug abuse and homosexual mode of transmission. Sixty-eight (49.63%) patients had CD4+ cell count recently, among them 23 (16.78%) had counts less than 250/μL and 45 (32.84%) had more than 250/μL. Most common HIV-related dermatological manifestations [Table 3] and [Table 4] were seborrheic dermatitis 89 (74.16%), xerosis 63 (52.5%), generalized skin hyperpigmentation 56 (46.67%), onychomycosis 53 (44.16%), pruritic papular eruption 27 (22.5%), oral candidiasis 21 (17.5%), photo dermatitis 21 (17.5%) and scabies 4 (3.33%). Statistically significant correlation with low CD4+ cell counts was found for oral candidiasis (P<0.0001) and Kaposi’s sarcoma (P 0.03); it was insignificant with other disorders like seborrheic dermatitis (P 0.22), xerosis (P 0.25) and onychomycosis (P 0.08).
| Table 2: Mode of transmission of HIV infection in patients
Click here to view |
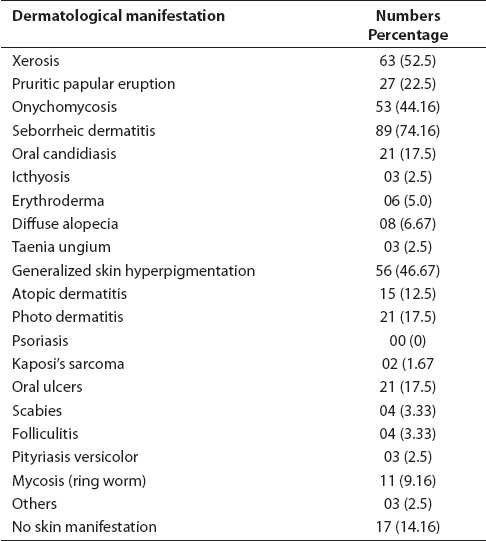 |
Table 3: Prevalence of dermatological manifestation in HIV-infected patients
Click here to view |
| Table 4: Cutaneous disorders and their correlation with CD4 cell count
Click here to view |
| Discussion |
Including many opportunistic infections, dermatological manifestations in HIV patients are very common. [8],[9] Results of the present study showed several facts about HIV in the tribal population of Bastar. Majority (90%) of the infected patients belonged to rural areas and lower socioeconomic strata (79.6%), with income less than Rs. 1500 per month. This indicates poor nutritional status, which itself can accelerate progression of HIV; 95.62% subjects were Hindus, probably due to the high density of the tribal Hindu population in this area. The predominant mode of transmission was heterosexual contacts (94.16%); this was unlike another study [18] which had reported that modes of transmission were 35.3% homosexual, 27.8% intravenous drug use and 24.4% heterosexual respectively.
The aim of the present study was to focus on dermatological manifestations in HIV-positive patients attending a tertiary care center (Government Medical College and Maharani Hospital, Jagdalpur) for treatment. We found 87.6% prevalence of dermatological disorders, which is high, similar to Jeffrey et al., [19] (86%) and Pitche et al., [20] (82.5%). Goodman et al., [16] reported higher prevalence whereas a south-western France study [18] showed it to be relatively lower (65.3%). Seborrheic dermatitis (74.16%) was the most common dermatological disorder in our study, like other studies [16],[21] where seborrheic dermatitis and candidiasis were most commonly present; the above-mentioned study [19] reported dermatophytosis as the most common manifestation. The second most common dermatologic manifestations in the present study were xerosis (52.5%) and generalized hyperpigmentation of skin (46.67%), much higher than previously reported studies [18],[19] 9.8% or 10.4% and (12%), respectively. Another common manifestation was onychomycosis (44.16%), also considerably higher than a similar study in South Western France (1.8%). Dermatological manifestations increase both in frequency and severity with progression of HIV and decline in CD4+ cell counts. There was a significantly high occurrence of oral candidiasis (P<0.0001) which was similar to many previous studies, [18],[22],[23] and of Kaposi’s sarcoma (P<0.03) amongst patients with low CD4+ counts (below 200/μl). We used diagnostic technique of clinical evaluation by a dermatologist rather than biopsy or scrapings for dermatological disorders. Despite following stringent criteria and taking all precautions to eliminate human errors, there may be a slight possibility of misdiagnosis in a few cases.
| Conclusion |
We concluded that the main mode of transmission of HIV in tribal regions is heterosexual contact; a critical factor facilitating infections is illiteracy/lack of knowledge and information regarding modes of spread of HIV. Dermatological manifestations have a high prevalence amongst HIV-positive subjects; of these, oral candidiasis and Kaposi’s sarcoma correlate significantly with low CD4+ counts. This may provide a clue to the diagnosis of HIV in patients reporting to the health providers, primarily for dermatological manifestations known to be associated with a decline in immune function. Thus, patients with such skin complaints may be motivated to report for voluntary counseling and treatment (VCTC). This also reiterates the need for thorough skin examination in HIV-positive patients, and provision of optimal medical care to these patients. Health education and information provided to people in these tribal areas so far has been insufficient and inadequate regarding modes of transmission and methods of prevention of HIV. This statement is truer, and sadly, so, for people from the lower socioeconomic strata and low educational status, another result emphasized in our study.
| Acknowledgment |
The authors would like to thank first and foremost Dr. SL Adile, Nodal Officer, and Director Medical Education, for all his support and guidance, without which this work could not have seen the light of day.
We shall also like to thank Dr. CS Kantarajan, Dean Government Medical College, Jagdalpur (CG), Dr. RR Sahni, Deputy Director, Health Services, Government of Chhattisgarh.
| References |
| 1. | UNAlDS, WHO, AIDS epidemic update, Dec 2006. |
| 2. | ASIA AIDS epidemic update Regional Summary Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization (WHO) 2008. Available from: http://data.unaids.org/pub/ [last cited on 2008]. |
| 3. | Estimated Adult HIV Prevalence, Statewise, India, 2006 HIV Sentinel Surveillance and HIV Estimation, 2006. National AIDS Control Organization (NACO), India. Available from: http://www.nacoonline.org/NACO [last cited on 2006]. |
| 4. | Categorisation of Districts based on HIV Sentinel Surveillance 2004, 2005 and 2006_Detailed List National AIDS Control Organization (NACO), India, Availble from: http://www.nacoonline.org/NACO [lasted cited on 2008 Sep 2]. |
| 5. | Bravo IM, Correnti M, Escalona L, Perrone M, Brito A,Tovar V, et al. Prevalence of oral lesions in HIV patients related to CD4 cell count and viral load in a Venezuelan population. Med Oral Patol Oral Cir Bucal 2006;11:E1-5. |
| 6. | Ranganathan K, Umadevi M, Saraswathi TR, Kumarasamy N, Solomon S, Johnson N. Oral lesions and conditions associated with Human Immu-nodeficiency Virus infection in 1000 South Indian patients. Ann Acad Med Singapore 2004;33:37-42. |
| 7. | Moniaci D, Greco D, Flecchia G, Raitieri R, Sinicco A. Epidemiology, clinical features and prognostic value of HIV-1 related oral lesions. J Oral Pathol Med 1990;19:477-81. |
| 8. | Wiwanitkit V. Prevalence of dermatological disorders in Thai HIV-infected patients correlated with different CD4 lymphocyte count statuses: A note on 120 cases. Int J Dermatol 2004;43:265-8 |
| 9. | Kumarasamy N, Solomon S, Madhivanan P, Ravikumar B, Thyagarajan SP, Yesudian P. Dermatologic manifestations among human immunodeficiency virus patients in south India. Int J Dermatol 2000;39:192-5. |
| 10. | Coopman SA, Johnson RA, Platt R, Stern R. Cutaneous disease and drug reactions in HIV Infection. N Engl J Med 1993;328:1670-4. |
| 11. | Tschachler E, Bergstresser PR, Sting lG. HIV-related skin diseases. Lancet 1996;348:659-63. |
| 12. | Uthayakumar S, Nandwani R, Drinkwater T, Nayagam AT, Darley CR. The prevalence of skin disease in HIV infection and its relationship to the degree of immunosuppression. Br J Dermatol 1997;137:595-8. |
| 13. | Goldstein B, Berman B, Sukeni KE, Frankel SJ. Correlation of skin disorders with CD4 lymphocyte counts in patients with HIV/AIDS. J Am Acad Dermatol 1997;36:262-4. |
| 14. | Smith KJ, Skelton HG, Yeager J, Ledsky R, McCarthy W, Baxter D, et al. Cutaneous findings in HIV-1 positive patients: A 42-month prospective study. J Am Acad Dermatol 1994;31:746-54. |
| 15. | Coopman SA, Johnson RA, Platt R, Stern RS. Cutaneous disease and drug reactions in HIV infection. N Engl J Med 1993;328:1670-4. |
| 16. | Goodman DS, Teplitz ED, Wishner A, Klein RS, Burk PG, Hershenbaum E. Prevalence of Cutaneous disease in patients with AIDS or AIDS-related complex. J Am Acad Dermatol 1987;17:210-20. |
| 17. | Coldiron BM, Bergstresser PR. Prevalence and clinical spectrum of skin disease in Patients infected with HIV. Arch Dermatol 1989;125:357-61. |
| 18. | Spira R, Mignard M, Doutre MS, Morlat P, Dabis F. Prevalence of Cutaneous Disorders in a Population of HIV-Infected Patients. Arch Dermatol 1998;134:1208-12. |
| 19. | Jeffrey HS, Muz P, Cabral P, Jhamb K. Dermatological manifestations in HIV-infected patients. Mayo Clin Proc 1999;74:658-60. |
| 20. | Pitche P, Tchangaï-Walla K, Napo-Koura G, Mijiyawa M, Agbere A, Tatagan A. Prevalence of skin disease in AIDS patients in the Lome-Tokoin Teaching Hospital of Togo. Sante 1995;5:349-52. |
| 21. | Coldiron BM, Bergstresser PR. Prevalence and clinical spectrum of skin disease in patients infected with human immunodeficiency virus. Arch Dermatol 1989;125:357-61. |
| 22. | Kolokotronis A, Kioses V, Antoniades D, Mandraveli K, Doutsos I. Immunologic status in patients infected with HIV with oral candidiasis and hairy leukoplakia. Oral Surg Oral Med Oral Pathol 1994;78:41-6. |
| 23. | Klein RS, Harris CA, Small CB, Moll B, Lesser M. Oral candidiasis in high-risk patients as the initial manifestation of Acquired immunodeficiency syndrome. N Engl J Med 1984;311:354-8. |
Source of Support: None, Conflict of Interest: None
| Check |
DOI: 10.4103/1755-6783.77188
| Tables |
[Table 1], [Table 2], [Table 3], [Table 4]



