| Abstract |
Staphylococcus aureus is an important causative organism for skin and soft tissue infection, which presents with the classical local signs of acute inflammation. Staphylococcal abscess without signs of inflammation (staphylococcal cold abscess) is a very rare entity, sometimes seen in immunocompromised host. Here, we report a case of a 50-year-old male patient who presented with bilateral asymptomatic cold abscess of staphylococcal origin over the anterior chest wall. The patient had no immunodeficiency and there was no distant/underlying source of staphylococcal infection. Smear and culture of pus proved the staphylococcal etiology and excluded tuberculosis, its close differential diagnosis. The patient was treated with antistaphylococcal antibiotics and local drainage of pus with complete recovery.
Keywords: Chest wall, cold abscess, skin and soft tissue infection, Staphylococcus aureus
| How to cite this article: Das SK, Das A, Dey S. A rare case of staphylococcal cold abscess of anterior chest wall in an immunocompetent adult. Ann Trop Med Public Health 2012;5:142-4 |
| How to cite this URL: Das SK, Das A, Dey S. A rare case of staphylococcal cold abscess of anterior chest wall in an immunocompetent adult. Ann Trop Med Public Health [serial online] 2012 [cited 2021 Mar 5];5:142-4. Available from: https://www.atmph.org/text.asp?2012/5/2/142/95977 |
| Introduction |
Localized collection of pus without signs of inflammation is called cold abscess. It is usually caused by tuberculosis, but can also follow actinomycosis, leprosy, and fungal infection. [1],[2],[3] Staphylococcus aureus is a highly virulent Gram-positive cocci, responsible for different Skin and Soft Tissue Infections (SSTI) such as folliculitis, boil, abscess, carbuncle, impetigo, and cellulitis. They are associated with the clinical features of acute inflammation originally described by Celsus, eg, calor (heat), rubor (redness), dolor (pain), and tumor (swelling). If these signs are lacking, staphylococcal cold abscess resembling tuberculous abscess develops. Recurrent staphylococcal cold abscess is an important feature of Hyperimmunoglobulin E Syndrome (HIES) or Job’s syndrome. [4] However, lack of inflammatory signs may also be a feature in patients with impaired immunity. Here, we report a case of staphylococcal cold abscess of the anterior chest wall in an immunocompetent patient. We report this case because of its rarity.
| Case Report |
A 50-year-old non-smoker, non-diabetic, non-hypertensive male farmer presented with bilateral, painless, soft tissue swellings over anterior chest wall of duration of 1 month. It was of insidious onset and progressively increasing in size. There was no fever, weight loss, or anorexia. There was no respiratory symptom. He was neither addicted to alcohol nor intravenous drugs. There was no history of similar swelling or tuberculosis in the past.
On general examination, there was no anemia, clubbing, or cervical or axillary lymphadenopathy. Skin in other parts of the body was normal. His oral temperature was 98.2°F, respiratory rate 16 breaths/min, pulse rate 82 beats/min, and blood pressure 110/70 mm Hg. There were two soft, nontender, fluctuant swellings with well-defined margins over both sides of the anterior chest wall. The right-sided swelling was lentiform in shape and 2 × 4 cm in size, while left-sided swelling was round and measured 3×5 cm. The swellings were not fixed to the overlying skin or underlying structures. There were no punctum or discharging sinus. Local temperature was not raised. Transillumination test was negative. The swelling were non-reducible, non-pulsatile, and there was no impulse on coughing.
Complete hemogram and blood biochemistry were within normal limit. A Chest X-Ray-Posteroanterior (CXR-PA) and left lateral view [Figure 1] revealed bilateral chest wall swellings without any pulmonary parenchymal or pleural abnormality. Result of Mantoux test (5 TU) was negative. Contrast-Enhanced Computed Tomography (CECT) thorax revealed bilateral swellings over anterior chest wall in the upper part without involvement of underlying bone, pulmonary parenchyma, or pleura; also, there was no adjacent lymphadenopathy or any spinal or paraspinal lesion [Figure 2]. Aspiration from non-dependent parts of both swellings revealed pus. Gram staining of pus showed Gram-positive cocci in clusters [Figure 3]. Ziehl-Neelsen stain (Z N stain) revealed no acid-fast bacilli. Aerobic culture of pus revealed growth of Staphylococcus aureus, while BACTEC culture of pus for Mycobacterium tuberculosis showed no growth. On drug sensitivity test, the strain was methicillin sensitive, and also sensitive to co-amoxiclav, piperacillin-tazobactam, cefuroxime, linezolid, vancomycin, and clindamycin. Blood cultures on two occasions were sterile. Anti-HIV-1/2 antibodies were negative. Serum Immunoglobulin (Ig)E was 420 IU/ml. Ultrasonography of whole abdomen revealed no abnormality. Echocardiography was within normal limit. A diagnosis of staphylococcal cold abscess was made on the basis of Gram stain and culture of the pus. He was treated with intravenous injection of co-amoxiclav 1.2 g thrice daily for 7 days, followed by oral co-amoxiclav 625 mg thrice daily for the next 7 days. Surgical incision and drainage of both swellings were also done. The patient made a complete uneventful recovery.
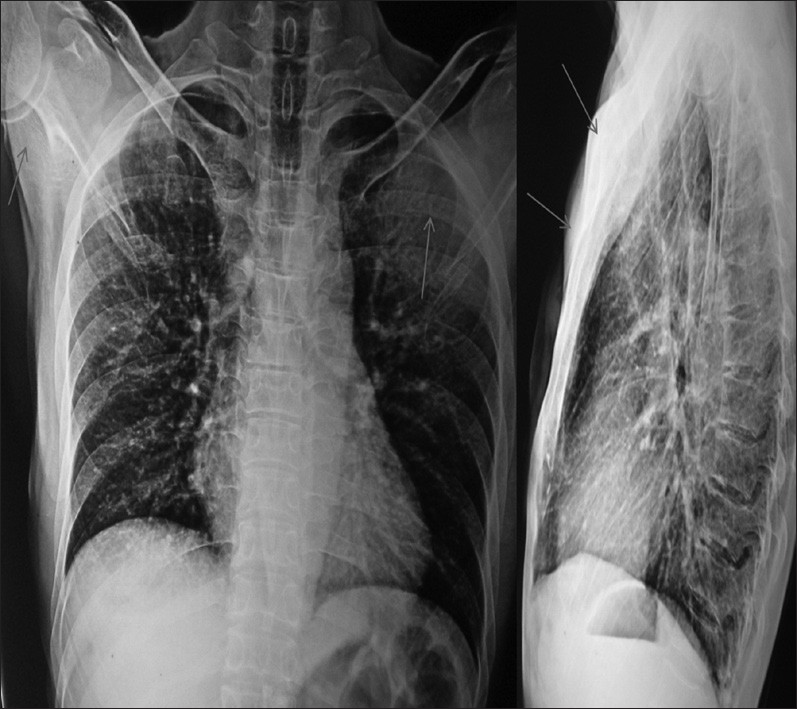 |
Figure 1: CXR-PA and lateral view showing bilateral swellings over chest wall
Click here to view |
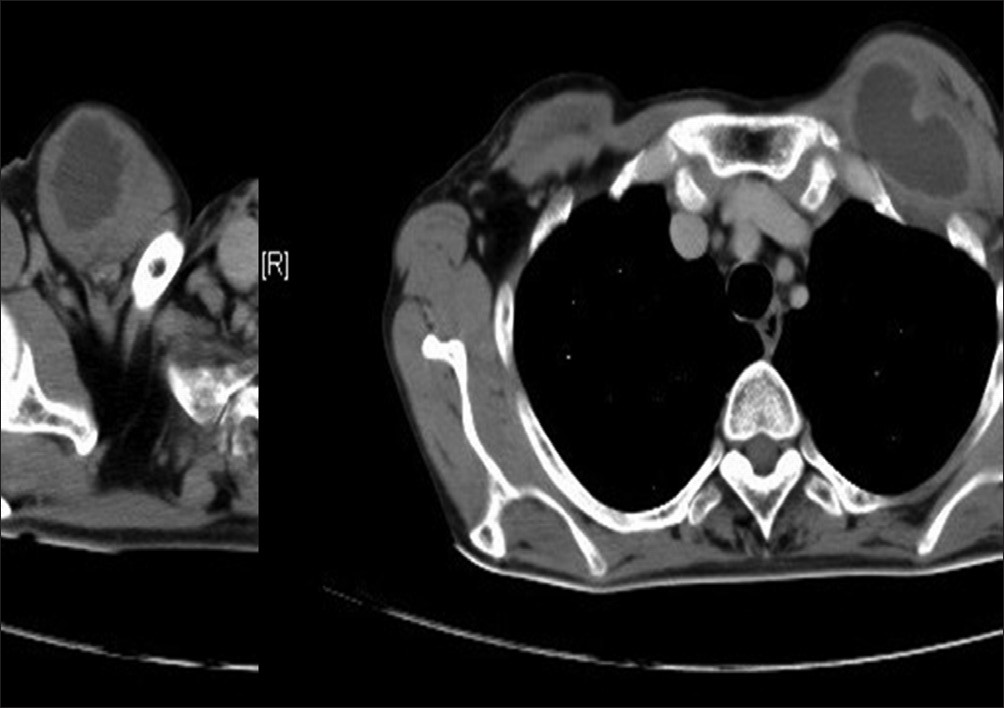 |
Figure 2: CECT thorax showing bilateral abscesses over anterior chest wall
Click here to view |
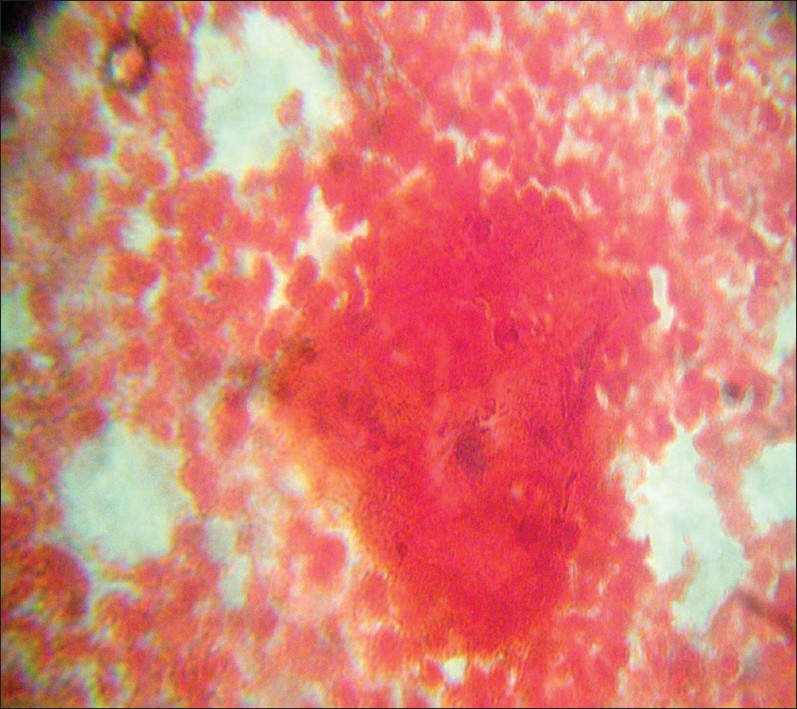 |
Figure 3: Gram stain showing numerous pus cells and Gram-positive cocci in clusters (100X)
Click here to view |
| Discussion |
Cold abscess is the classical manifestation of tuberculosis. It develops so slowly that there is very little inflammation. Cold abscess commonly develops secondary to tuberculosis of the spine, hip, or lymph node. Cold abscess in the chest wall generally originates from vertebral tuberculosis or from tuberculosis of lymph nodes in the posterior mediastinum or the internal mammary group of lymph nodes. Tuberculous exudates from the spine generally follow the course of anterior cutaneous or lateral cutaneous branch of the intercostal nerve to produce cold abscess in the parasternal line or midaxillary line, respectively. Cold abscess in the chest wall can also be a consequence of spontaneous decompression of tuberculous empyema by dissecting through the chest wall producing ’empyema necessitans’. [5] Nontuberculous cold abscess is relatively rare, but has been documented in a variety of clinical situations. [6],[7],[8]
Staphylococcal abscess generally presents with florid signs of local inflammation. However, staphylococcal cold abscess may be present in patients in immunocompromised state like diabetes mellitus, neutropenia, chronic granulomatous disease, Job’s syndrome, etc. Recurrent staphylococcal cold abscess is classically seen in Job’s syndrome, which also includes eczematoid dermatitis, severe staphylococcal pneumonia and very high concentration of serum IgE (>2,000 IU/ml). The cold abscess in this syndrome has been thought to be due to defective neutrophil chemotaxis, which, in turn, may result directly or indirectly from the interaction of the antigen (Ig) and sensitized leukocytes. [9] There has been rare reports of staphylococcal cold abscess in an immunocompetent host. [10]
Tuberculous etiology of our patient was excluded from the negative Z N stain, negative tuberculous culture of the pus, and absence of evidence of spinal, mediastinal nodal, or pleural tuberculosis in CT scan of thorax. Suggestive Gram stain and positive culture established the staphylococcal origin of the abscess. Normal fasting plasma glucose and normal blood count excluded diabetes mellitus and neutropenia, respectively. Absence of other suggestive features, and normal IgE level excluded Job’s syndrome. Therefore, our case appeared to be a unique one, where staphylococcal cold abscess developed in an immunocompetent adult without any obvious defect in his immune system.
| References |
| 1. | Faure E, Souilamas R, Riquet M, Chehab A, Pimpec-Barthes FL, Manac’h D, et al. Cold abscess of the chest wall: A surgical entity? Ann Thorac Surg 1998;66:1174-8. |
| 2. | Leafstedt SW, Gleeson RM. Cervicofacialactinomycosis. Am J Surg 1975;130:496-8. |
| 3. | Thomas M, Emmanuel M. Facial nerve abscess in a case of leprosy: A case report. Neurol Asia 2009;14:41-2. |
| 4. | Davis SD, Schaller J, Wedgwood RJ. Job’s syndrome: Recurrent ‘cold’ staphylococcal abscess. Lancet 1966;1:1013-5. |
| 5. | Porcel JM, Madronero AB, Bielsa S. Tuberculous empyema necessitatis. Respiration 2004;71:191. |
| 6. | Lee SS, Chan YS, Chen CY, Fu TS, Ueng SW. Nontuberculous cold abscess of psoas muscle:An unusual manifestation of colocutaneous fistula. Arch Orthop Trauma Surg 2000;120:224-5. |
| 7. | Huber F, Leaute-Labreze C, Lina G, Sarlangne S, Taieb A, Boralevi F. Multiple neonatal staphylococcal cold abscess of the large folds. J Eur Acad Dermatol Venerol 2006;20:1197-2000. |
| 8. | Miech G, Morand G, Witz JP. Cold abscess of the thoracic wall due to echinococcosis. Poumon Coeur 1972;28:543-4. |
| 9. | Hill HR. Defect in neutrophil granulocyte chemotaxis in Job’s syndrome of recurrent ‘cold’ staphylococcal abscesses. Lancet 1974;304:617-9. |
| 10. | Rosenfeld LE. Osteomyelitis of the first rib presenting as cold abscess nine months after subclavian venous catherization. Pacing Clin Electrophysiol 1985;8:897-9. |
Source of Support: None, Conflict of Interest: None
| Check |
DOI: 10.4103/1755-6783.95977
| Figures |
[Figure 1], [Figure 2], [Figure 3]



