| Abstract |
Though the incidence of tuberculosis is high in India, primary tuberculosis of breast is extremely rare. Tuberculosis of breast often mimics breast cancers clinically. We are reporting here five cases of primary tuberculosis of breast presented with painless breast lumps. Diagnosis was done by fine-needle aspiration cytology (FNAC) of breast lump by the presence of epitheloid cell granulomas, caseation, Langhan’s type of giant cells and in two cases by the presence of acid-fast bacilli. All these cases responded to six month anti-tuberculosis regimen.
Keywords: Breast, fine-needle aspiration cytology, tuberculosis
| How to cite this article: Bhosale AA, Joshi AR, Ashturkar AV, Pathak GS. Primary tuberculosis of breast: A case series. Ann Trop Med Public Health 2012;5:262-4 |
| How to cite this URL: Bhosale AA, Joshi AR, Ashturkar AV, Pathak GS. Primary tuberculosis of breast: A case series. Ann Trop Med Public Health [serial online] 2012 [cited 2020 Aug 10];5:262-4. Available from: https://www.atmph.org/text.asp?2012/5/3/262/98634 |
| Introduction |
Tuberculosis (TB) of breast is extremely rare even in developing countries where pulmonary and other forms of extrapulmonary manifestations of TB are endemic. [1] Breast tissue, along with skeletal muscle and spleen, appears to be relatively resistant to tuberculous infection. [2] Incidence of breast TB accounts for less than 0.1% of all breast lesions in Western countries and 4% of all breast lesions in TB endemic countries. [3],[4] The clinical signs of mammary TB can be insidious and nonspecific and often simulate signs of breast carcinoma. Mammary TB usually affects young, multiparous and lactating women and rarely in male patients. [5]
Histopathological examination using fine-needle aspiration cytology (FNAC) may reveal caseating epitheloid cell granulomas and acid-fast bacilli (AFB). Although the presence of an acid-fast stain or culture is essential to confirm the diagnosis, it does not give a positive result in most patients. [4] Here we report five cases of primary breast TB diagnosed primarily by FNAC and treated with anti-TB chemotherapy.
The aim of this study is to highlight the importance of FNAC in the diagnosis of breast TB, which can be easily managed conservatively, thus saving the patient from unnecessary invasive interventions.
| Case Report |
All five patients in our series were women with an age ranging from 24 to 41 years. These patients presented with painless lump in the breast of 1 to 3 months duration. There was no history of nipple discharge, fever, weight loss or cough. Physical examination revealed firm irregular breast lump adherent to overlying skin. In three cases, lump was located in subareolar region, and in remaining two cases, it was located in the upper outer quadrant. There was no evidence of axillary lymphadenopathy. On routine investigations, hemogram and biochemical tests were normal except for elevated erythrocyte sedimentation rate (ESR). Mammographically, the lesions appeared as ill-defined, dense, round to oval densities, without microcalcification. On this basis, clinical diagnoses of pyogenic abscess and malignancy were kept in the mind.
Patients were subjected for FNAC to rule out malignancy. The aspirates yielded purulent, hemorrhagic material. Initially, the cytological smears were stained with Leishman stain and hematoxylin and eosin (H and E) stains.
The smears revealed few ill-defined epithelioid cell granulomas with occasional Langhan’s type of giant cells and lymphocytes. Singly scattered ductal epithelial cells were also seen. The background revealed predominantly granular necrotic material [Figure 1] and [Figure 2]. On Ziehl-Nielson (ZN) stain, two cases were positive for AFB [Figure 2]. Focus of TB elsewhere in the body was ruled out by detailed clinical examination, chest X-ray and abdominal ultrasonography. On this basis, all these patients were started on standard six-month anti-TB regimen (isoniazid, rifampicin, pyrazinamide and ethambutol), with good clinical response in the form of resolution of mass. On regular follow-up, all these patients have been asymptomatic and there is no recurrence.
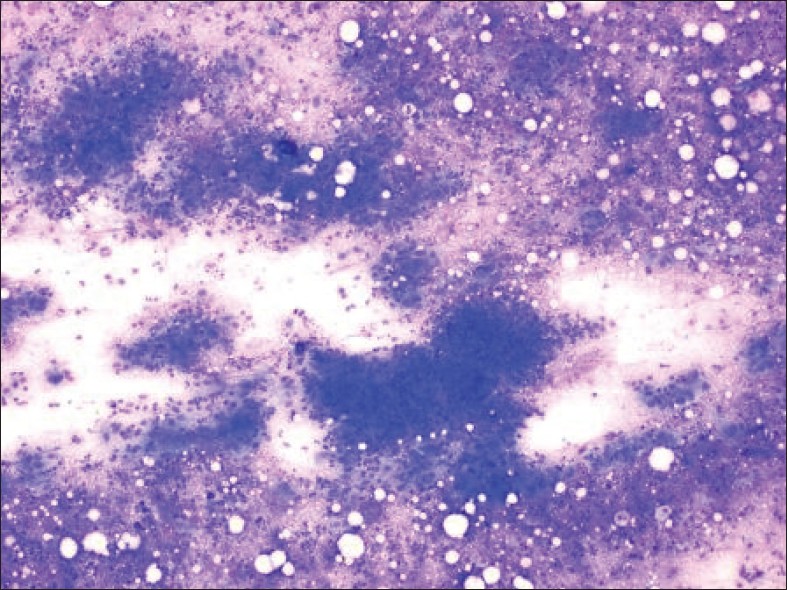 |
Figure 1: Photomicrograph of smear from breast aspirate showing epithelioid cell granulomas with caseous necrosis and singly scattered ductal epithelial cells in the background (Leishman stain 4x) |
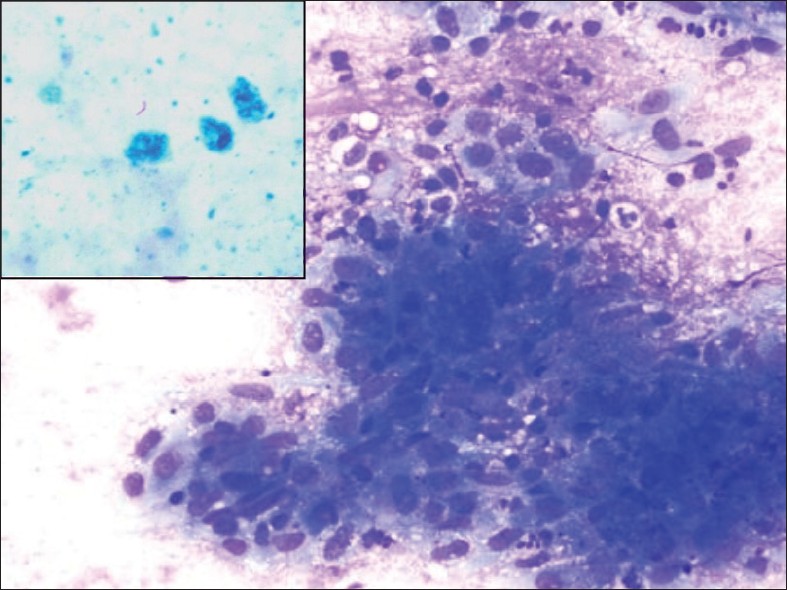 |
Figure 2: Photomicrograph shows closer view of epitheloid cell granuloma (Leishman stain 10x). Insert shows presence of acid-fast bacilli (Z-N stain 100x) |
| Discussion |
TB of the breast is an extremely rare disease. It was first described by Sir Astley Cooper in 1829 as, “scrofulous swelling in the bosom of young women”. [6] In developing countries, where TB is endemic, the incidence is 0.25-4.5%. It is usually suspected in a multiparous, lactating woman who may be immunocompromised. [6] However, a recent increase in incidence has been observed, both in developed and developing countries, which is thought to relate to migration from endemic areas and the increase in the number of immunocompromised patients. [7] It can be classified as primary or secondary. [8] Primary involvement is tuberculous infection confined only to the breast and is extremely uncommon. [8] Secondary involvement is when there is co-existing tuberculous lesion elsewhere in the body. [8] In the present study, all the patients were immunocompetent; also there was no focus of TB elsewhere in the body.
TB of the breast is usually a disease of women aged between 20 and 50 years. [9] All the patients in our series were middle aged. The mode of disease transmission can be haematogenous or by direct extension after contact with infected material through abrasions of the skin of the lactiferous ducts. [9] The typical patient is a young woman with a fluctuant central breast abscess or a firm poorly defined mass with associated skin or nipple retraction, suggestive of carcinoma. Purulent discharge from the nipple is common. Fistulas and sinus tracts occur in advanced disease. [9] The disease presents as an irregular lump in the breast, sometimes fixed to the overlying skin or underlying muscle and is often overlooked and misdiagnosed as carcinoma or pyogenic abscess. [10] In our case series, breast lumps were located in central and upper outer quadrant with adherence to overlying skin and clinically mimicking malignancy.
Radiological imaging modalities like mammography or ultrasonography are unreliable in distinguishing it from carcinoma because of the variable pattern of presentation of such an inflammatory lesion. [11] Diagnosis is ideally by demonstration of AFB in the breast tissue by Ziehl-Neilson stain or culture. [12],[13] However, the bacilli are isolated in only 25% of cases, therefore demonstration of caseating granulomas from the breast tissue and involved lymph nodes is usually sufficient for the diagnosis. [12],[13] In the present study, only two cases revealed presence of AFB. Remaining cases were diagnosed as TB on the basis of epitheloid granulomas and caseous necrosis in the background. Sharma et al. [14] reported seven cases of TB of breast with multiple discharging sinuses, lump, ulcer and recurring abscess of breast. Diagnosis of TB was based on histological appearance, AFB being detected in only one case. Successful treatment combines antituberculous drug therapy with removal of infected breast tissue. According to Hamit [2] in 60% of cases it may not be possible to recover AFB from any site, including the breast. However, TB should be suspected in a patient who has a recurring breast abscess after adequate drainage on previous occasions. Molecular detection of Mycobacterium TB by polymerase chain reaction can be particularly useful in the validation of a diagnosis of TB in clinical settings, where the diagnosis is uncertain. [4]
In our study all five patients responded to six months standard anti-TB therapy without any recurrence. Treatment of breast TB with standard anti-TB therapy for 6 months usually results in good clinical response. The regimen consists of a two-month intensive phase (isoniazid, rifampicin, pyrazinamide and ethambutol), followed by a four-month continuation phase (isoniazid and rifampicin). [4],[15] Surgical intervention is indicated in cases showing poor response to anti-TB therapy, and is reserved for draining cold abscesses or excision of residual lumps. Simple mastectomy is reserved for cases with extensive disease causing a large painful ulcerated mass involving the entire breast. [4],[15]
In country like India, where TB is endemic, caseous necrosis with epitheloid cell granulomas even in absence of AFB should alert one to the diagnosis of TB. Only after sufficient trial of anti-tuberculous treatment has been given without expected response, should an alternative diagnosis be suggested.
| Conclusion |
To conclude, breast TB is an obscure disease often mistaken for carcinoma or pyogenic abscess, especially if well-defined clinical features are absent. Thus, a high index of suspicion is essential as the disease can be treated conservatively with current anti-TB modalities.
| References |
| 1. | Alagaratnam TT, Ong GB. Tuberculosis of the breast. Br J Surg 1980;67:125-6. |
| 2. | Hamit HF, Ragsdale TH. Mammary tuberculosis. JR Soc Med 1982;75:764-5. |
| 3. | Akcakaya A, Eryilmaz R, Sahin M, Ozkan O: Tuberculosis of the breast. Breast J 2005;11:85-6. |
| 4. | Tewari M, Shukla HS. Breast tuberculosis: Diagnosis, clinical features and management. Indian J Med Res 2005;122:103-10. |
| 5. | Jaideep C, Kumar M, Khanna AK. Male breast tuberculosis . Postgrad Med J 1997;73:428-9. |
| 6. | Kaneria MV, Sharbidre P, Burkule D, Shukla A, Somani A, Nabar ST. Bilateral breast tuberculosis: A rare entity. J Indian Acad Commun Med 2006;7:61-3. |
| 7. | Yuen JH, Lam TP, Leong L. Primary tuberculosis of the breast. J HK Coll Radiol 2003;6:33-5. |
| 8. | Gupta PP, Gupta KB, Yadav RK, Agrawal D. Tuberculous mastitis: A review of seven consecutive cases. Indian J Tuber 2003;50:47. |
| 9. | Hale JA, Peters GN, Cheek JH. Tuberculosis of the breast: Rare but still existent: Review of the literature and report of an additional case. Am J Surg 1985;150:620-4. |
| 10. | Maroulis I, Spyropoulos C, Zolota V, Tzorakoleftherakis E. Mammary tuberculosis mimicking breast cancer: A case report. J Med Case Rep 2008;2:34. |
| 11. | Khanna R, Prasanna GV, Gupta P, Kumar M, Khanna S, Khanna AK. Mammary tuberculosis: Report on 52 cases. Postgrad Med J 2002;78:422-4. |
| 12. | Kakkar S, Kapila K, Singh MK, Verma K. Tuberculosis of the breast: A cytomorphologic study. Acta Cytol 2000;44:292-6. |
| 13. | Gupta D, Rajwanshi A, Gupta S, Nijhawana R, Saran RK, Singh R. Fine needle aspiration cytology in the diagnosis of tuberculosis mastitis. Acta Cytol 1999;43:191-4. |
| 14. | Sharma PK, Babel AL, Yadav SS. Tuberculosis of breast (study of 7 cases). J Postgrad Med 1991;37:24-6,26A. |
| 15. | Sriram KB, Moffatt D, Stapledon R. Tuberculosis infection of the breast mistaken for granulomatous mastitis: A case report. Cases J 2008;1:273. |
Source of Support: None, Conflict of Interest: None
| Check |
DOI: 10.4103/1755-6783.98634
| Figures |



