Context: Human immunodeficiency virus (HIV) infection and resulting immune depression are associated with increase proportions of extrapulmonary tuberculosis (EPTB). The prevalence of EPTB varies across studies between 15 and 50% and depends on the region, ethnic group studied, and HIV coinfection rates. In Cameroon, no studies have been done so far to evaluate the magnitude of this form of tuberculosis (TB), the various sites involved, and their association with HIV infection. Aims: To determine the prevalence of EPTB, the various organ sites affected and their association with HIV infection in a population of patients treated for TB. Settings and Design: We did cross-sectional analysis of the data from the TB register of the Douala General Hospital, a tertiary health institution situated in Douala, Cameroon. All cases of TB diagnosed between 1 st July 2007 and 30 th June 2011 were included. Results: Of total of 749 patients recorded for anti-TB treatment, the overall prevalence of HIV was 41.5% (95% confidence interval [CI]38-45.1). The prevalence of EPTB was 42.9% (321). HIV infection was present in 33.6% of patients with EPTB. The most affected sites of disease were bones and joints (29.6%), lymph nodes (17.8%), the pleura (15%), peritoneum (14.3%), and the central nervous system and meninges (9%). Neuromeningeal TB however, less common was most strongly associated with HIV infection, odd ratio (OR)2.3 (95% CI 1.1-5.0, p < 0.05). Conclusions: The proportion of EPTB among TB patients treated in the Douala General Hospital is relatively high with bone and joints being the most affected sites. HIV infection is most strongly associated with neuromeningeal forms. Keywords: Bone and joints tuberculosis, extrapulmonary tuberculosis, human immunodeficiency virus coinfection, neuromeningeal tuberculosis
Tuberculosis (TB), which is one of the three largest single-agent cause of infectious diseases [1] (along with malaria and human immunodeficiency virus [HIV]), is a global public health problem due to its high morbidity and mortality. At present, it is estimated that at least one third of the human population is infected by Mycobacteriumtuberculosis.[1] The World Health Organisation (WHO) estimated a global incidence of active TB in 2009 at 9.4 million cases and a prevalence of 14 million cases. [1] About 11-13% of these incident cases were among HIV-infected persons. [1] This is because HIV-associated immune depression increases the risk of active TB from about 5% in a lifetime to 10% per year. [2] Although this risk depends on the degree of immune depression, prevailing socioeconomic conditions, and risk of TB exposure, high burden of HIV in Sub-Saharan Africa [3] accounts for4of 5HIV-associated TB in the world [1] with rates of up to 30% per year among those with low CD4 counts. [4] Although TB is acquired by inhalation of contaminated droplets, it can produce disease in any organ system other than the lungs, which is usually the initial site of infection.With this increase awareness on the burden of TB, there has been an increase in the number of reported cases of extrapulmonary tuberculosis (EPTB), and depending on the region, ethnic group, and HIV coinfection rates, the prevalence of EPTB is between 15 and 50%. [5] This increase in the proportion of cases of EPTB may reflect either an improved ability for detection or an increased survival of immune suppressed people and the likelihood of TB reactivation at various sites. Compared withHIV-uninfected person in whom EPTB accounts for about 20% of TB, HIV-infected persons are more prone to EPTB in whom it accounts for 53-62% of TB cases. [6] The term EPTB, which encompasses all forms of TB other than pulmonary TB (PTB), has a broad spectrum of clinical manifestations, hence a real diagnostic challenge. [7] The diagnosis whose confirmation reposes on obtaining material for culture is much more difficult [5] and technically more demanding than for PTB. In Cameroon, where the prevalence of HIV is estimated at 5.3% of the adult population, [3] annual incidence of TB is estimated at 177 per 100,000 people per year. [1] Although estimated HIV-TB coinfection rates approach 50%, [8],[9] there is no published data on the association between HIV and EPTB whose diagnosis is still very uncommon among many physicians. To bridge this information gap, we decided to determine the prevalence of EPTB, the various organ sites affected, and their association with HIV infection in a group of patients receiving anti-TB treatment at the Douala General Hospital.
Study setting The study was undertaken at the Douala General Hospital, a tertiary health facility in Douala, the economic capital city of Cameroon. In this hospital, all patients diagnosed with TB are registered in a TB register before commencement of therapy. The diagnosis of TB is based on the guidelines of the National Tuberculosis Control Programme. [10] Smear-positive PTB is diagnosed on the basis of a suggestive clinical history and the presence of acid-fast bacilli (AFB) on at least one of the three smears prepared from three sputum samples submitted on three consecutive days for microscopic examination after staining by Ziehl-Neelsen’s technique. The diagnosis of smear-negative PTB is retained for a patient with clinical signs and symptoms suggestive of the disease despite the negativity of the first series of sputum examinations, no improvement after a 10-day course of nonspecific antibiotic therapy, persistent negative results of a new series of two sputum smear examinations, no evident course of the disease, and a chest X-ray image suggestive of PTB. The diagnosis of EPTB lies for the most part on the clinical decision based on suggestive clinical signs and evidence of a predominantly lymphocytic exudate as in the case of peritoneal TB with ascites or granulomatous lesions on histopathological examination of lymph nodes or other pieces of tissue obtained by biopsy. Patients with PTB associated or not with extrapulmonary sites are considered pulmonary cases and recorded as such. No mycobacterial cultures are done in this hospital due to logistic reasons. In the Douala General Hospital also, all patients diagnosed with TB are offered voluntary counseling and testing (VCT) for HIV in accordance with the National AIDS Control Programme in Cameroon. [11] HIV antibodies are detected using a third-generation enzyme-linked immunosorbent assay (ELISA) test BIOREX® (Biorex Diagnostics Limited, Antrim, United Kingdom). If the test is positive, a second sample is collected for a second ELISA which if positive, a third test Genie® III HIV-1/HIV-2 Assay (Bio-Rad Diagnostics, Marnes La Coquette, France) is done which distinguishes HIV 1 from HIV 2. When the three tests are positive, the patient is considered positive for HIV. In case of a discordant result, a confirmation test is carried out by the Western blot technique (New LAV blot, Diagnostics, Pasteur, Marnes La Coquette, France). The results of this test are also recorded in the TB register. Methods All patients consecutively diagnosed with TB at the Douala General Hospital from July 1, 2007 to June 30, 2011, were studied. The diagnosis for each patient was obtained through a thorough review of the TB register and the consultation register of the internal medicine unit. Information on age, sex, HIV serostatus, and form of TB (pulmonary or extrapulmonary) and if extrapulmonary, organ or structure affected, was extracted for each patient and recorded in a pre-prepared data collection form. Information on CD4 count of HIV-positive patients was not included in the analysis because it was not available in the records used. Data analysis Data analysis was done using STATA11.2 statistical software (Stata Corporation, College Station, Texas). We expressed our results as proportions of total populations and used the Pearson Chi-square test to compare proportions. For univariate analysis, we used Mantel-Haenszel method and reported results as odd ratio (OR) together with their 95% confidence intervals (CI). A two-tailed P-value with cut-off of significance of less than 0.05 was used.
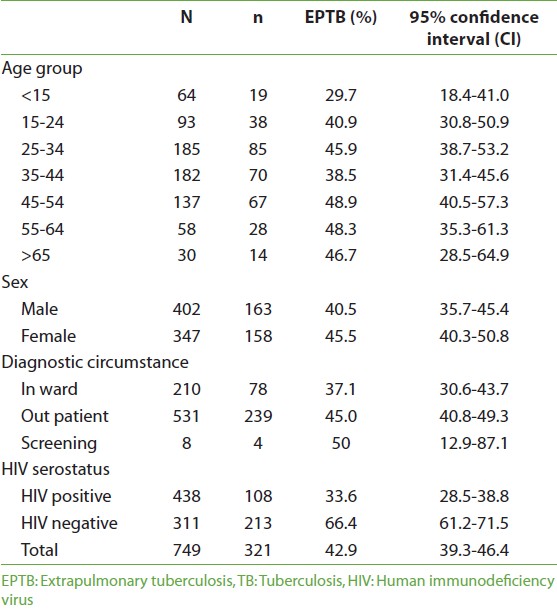
During the study period, a total of 749 patients were recorded for anti-TB treatment of whom 53.8% (402) were men. The overall prevalence of HIV in this population was 41.5% (95% CI38-45.1) and was similar in both sexes: OR 1.2 (95%CI0.7-1.9, P > 0.05). Of the total population, 42.9% (321) were diagnosed with EPTB [Table 1]. Their mean age was 37.8±15.6 years.
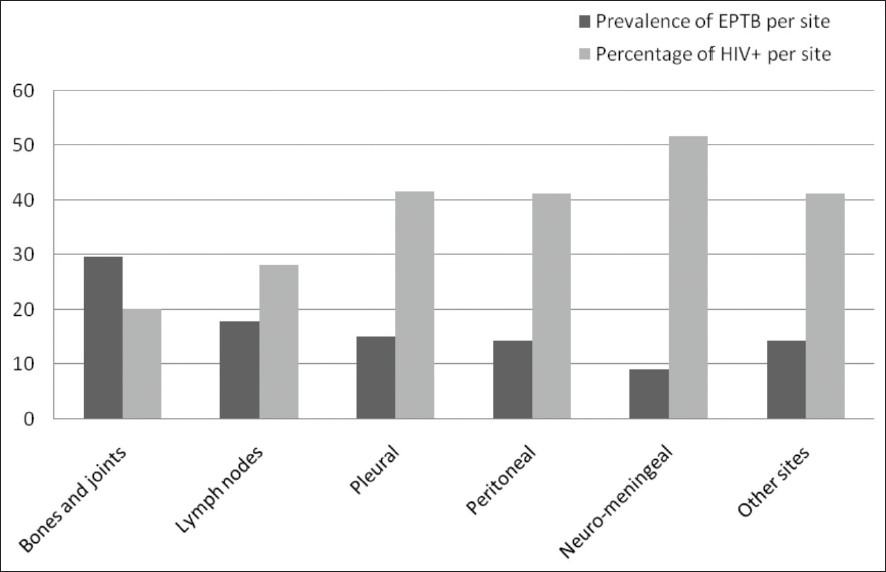
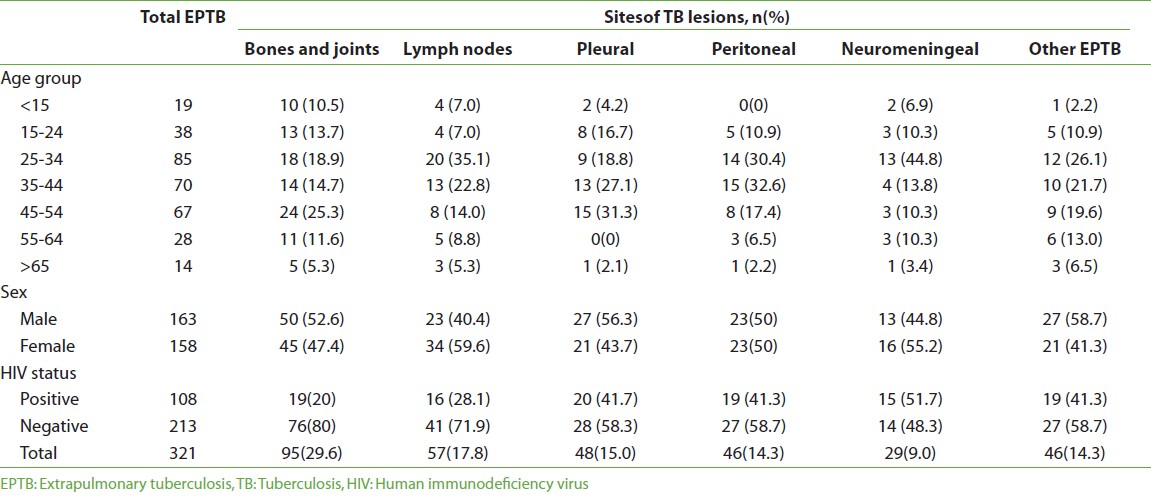
The prevalence of HIV among these patients with EPTB was 33.6% (95% CI 28.5-38.8) [Table 1], with no statistically significant difference between men and women (OR 1.2, 95%CI 0.7-1.9, P = 0.5). However, patients with PTB were more likely to be HIV seropositive than those with EPTB, OR 1.8 (95% CI 1.3-2.4, P = 0.001). There was no association between age, TB diagnostic circumstances, and HIV-positive serostatus (OR 1.1 and 0.9, respectively, P > 0.05). The most common extrapulmonary site of TB lesions was bones and joints in 29.6% (95) of patients [Table 2], [Figure 1], and the least common was neuromeningeal TB in 9% (29) of patients [Table 2]. Other sites that included TB of the skin, bladder, and genitals were found in 14.3% (46) of patients.
Bone and joint TB, although the most prevalent, had the lowest prevalence of HIV [Figure 1]. Although pleural and peritoneal TB were associated with HIV, neuromeningeal TB had the highest prevalence of HIV, and compared with all other EPTB sites, it was strongly associated with HIV-positive serostatus, OR 2.3 (95% CI 1.1-5.0, P = 0.03). Most (44.8%) of those with neuromeningeal TB were between the age group of 25and 34 years [Table 2]. After adjusting for age, neuromeningeal TB still remained strongly associated with HIV-positive serostatus (adjusted OR 2.7, 95%CI 1.1-6.5, P = 0.02)
Our study which was aimed at determining the prevalence of EPTB, the various organ sites involved, and their association with HIV in patients registered for anti-TB treatment in the General Hospital Douala was done by a cross-sectional analysis. We chose this study design because it was the most suitable means of attaining our objectives using this registered information. A prevalence of EPTB of 42.9% in our study is quite high compared with a recent finding of EPTB of 17% in Yaoundé the capital city of Cameroon. [12] This difference might be due to the fact that the study in Yaoundé was carried out in the chest unit of a reference hospital, and the patients with EPTB could have been those with associated PTB. Our finding is, however, similar to what was found in Nepal in 2008 [13] and in India in 2006, [14] which are settings with similar TB burden like ours. Relatively lower prevalence of 20-25% was found in Iran and in many areas of the United States, [5],[15],[16] which are areas with lower TB burden. However, in some areas with low TB burden, the prevalence among African and Asian immigrants was similar to ours [17] and therefore might be reflecting the burden of EPTB in the country of origin of these immigrants. Furthermore, in our study, this prevalence could as well be an underestimation as patients with both PTB and EPTB were all recorded in the TB register as PTB. We found bones and joints to be the most common site affected. This was very different from what has been reported in many different studies where lymph node involvement was the most common site of infection. [17],[18],[19],[20],[22] This finding simply reflects the reality of our study setting which happens to harbor the largest rheumatology, neurology, and orthopedic reference units of the subregion where most patients with joint and bone diseases are referred including those with TB-related causes. Also in Douala, there is a big TB diagnostic and treatment center with chest physicians who provide a cheaper service. This may therefore lead to a selection bias. Nevertheless, lymph node and pleural involvements were the next main sites of infection in our study, similar to other studies. [17],[18] HIV prevalence in our study was 33.6% in patients with EPTB, and even higher among patients with PTB. Even so, this high coinfection rate could be explained by the fact that Cameroon is situated in a region with a high burden of both infections compared with other regions like the United States of America. [5],[16],[23] However, our finding of higher HIV prevalence among PTB patients might be because in our institution, patients with both PTB and EPTB are registered as having PTB. Given evidence shows that EPTB is more associated with HIV, [24] and the EPTB-HIV co-infected patients registered as having PTB might have contributed to this high PTB-HIV coinfection rate that we found. Either way, HIV and TB coinfection rates are high in Cameroon. Neuromeningeal TB was the least common in our study with a prevalence of 9%. This finding is lower than that of a recent American study which reported a prevalence of neuromeningeal TB of 22% among patients with EPTB. [25] We also found that neuromeningeal TB compared with other TB sites was strongly associated with HIV infection. This finding is in line with what leeds and collaborators found where they showed that HIV infection especially with a low CD4 count of <100 cells/ml was a factor associated with severe forms of EPTB among which neuromeningeal and disseminated. [25] Given that we did not include CD4 cell count in our analysis, we cannot predict whether this association in our population increases with severity of immune depression. There were certain limitations to our study. First, being a hospital-based study in an institution with many specialties which are not available in other hospitals in the same town, there was some selection bias of our study population and our finding might not really reflect the reality of EPTB in Cameroon. Second, being an observational study from hospital registers, analysis was limited only to the variables available in these registers. That notwithstanding, we have shown that the prevalence of EPTB among patients on TB treatment is high with bones and joints being the most affected sites. Central nervous system and meningeal TB were strongly associated with HIV infection. Our study therefore gives some perspective of EPTB and HIV coinfection in Cameroon thereby setting a platform for more studies. Furthermore, our findings might help reinforce the need for integrated management of HIV and TB in Cameroon, which is mandatory for the global fight against TB.
Source of Support: None, Conflict of Interest: None
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||