| Abstract |
Background: Polycystic ovarian syndrome (PCOS) is the most frequent endocrinological disorder affecting young women of reproductive age having wide spread morbidity. Though, several factors have been identified attributing to its cause, yet it demands further investigations. Materials and Methods: A community-based cross-sectional study was carried out among 253 adolescent females (age: 10-19 years) to elicit the associations between PCOS and the cesarean mode of delivery, eruption of wisdom tooth and other factors through a binary logistic regression analysis. Results: The mean age was 18.57 0.19 (standard error of mean) years. The prevalence of PCOS in Nellore district is 15.4% (95% confidence interval: 10.97-19.83). Higher risk of PCOS was associated with the cesarean mode of delivery (odds ratio [OR] = 4.91, P < 0.0001), eruption of at least 1 wisdom tooth (OR = 2.61, P = 0.025) and the presence of central obesity (OR = 2.57, P = 0.05). Discussion: An attempt has been taken to hypothesize causal association of associated factors with PCOS from the available literature, which in turn may pave the path for newer approaches for prevention and management.
Keywords: Cesarean, migration, obesity, wisdom tooth
| How to cite this article: Bhuvanashree N, Gupta S, Anitha M, Venkatarao E. Polycystic ovarian syndrome: Prevalence and its correlates among adolescent girls. Ann Trop Med Public Health 2013;6:632-6 |
| How to cite this URL: Bhuvanashree N, Gupta S, Anitha M, Venkatarao E. Polycystic ovarian syndrome: Prevalence and its correlates among adolescent girls. Ann Trop Med Public Health [serial online] 2013 [cited 2021 Mar 6];6:632-6. Available from: https://www.atmph.org/text.asp?2013/6/6/632/140233 |
| Introduction |
Polycystic ovarian syndrome (PCOS) is the most frequent endocrinological disorder affecting 5-10% of women in the reproductive age. [1] Its wide continuum of clinical manifestations such as oligomenorrhea, cosmetic deformities such as hirsutism, alopecia, obesity [2] and the impending fear of infertility with the anxiety of future metabolic complications has a remarkable impact over the psychology, [3],[4] of the young women. Further, it is associated with a wide spectrum of morbidity, [1],[5] including cardiovascular abnormalities, type 2 diabetes mellitus, dyslipidemia, risk of malignancies and infertility. [6],[7] Many environmental, ethnic, clinical and genetic, [6],[7],[8] causes have been attributed for its etiopathology, yet it demands further investigation in understanding the disease, which in turn will open new gateways for prevention and treatment.
It was an accidental observation by the authors that most of the cases who suffered from PCOS were delivered through the cesarean section, they had erupted at least one wisdom tooth and had migrated at least once after attaining menarche. This prompted to conduct a community-based, cross-sectional observational study in the adolescent females to estimate the strength of association of PCOS with the mode of delivery, eruption of wisdom tooth, migration and other variables. The study was approved by the institutional ethical committee and all diagnosed cases were provided specialist consultation.
| Materials and Methods |
Study setting
Nellore, in Andhra Pradesh, India is an educational hub that hosts students from different parts of the state. Various schools, colleges and hostels of the town and the adjacent rural areas were visited to recruit the study subjects. The study was conducted during the period April and May 2010 as a short-term studentship research project of Indian Council of Medical Research.
Selection of study subjects
An informed written consent was obtained prior to conducting the study. In case an individual being lesser than 18 years, consent was obtained from the parent/guardian. Girls who have not attained menarche were excluded. The girls were addressed in small groups of not more than 30 individuals.
A total of 300 adolescent girls of age 10-19 years were approached. Among them, 253 cooperated and completed the questionnaire and physical examination with a non-response rate of 15.6%. The subjects were selected randomly from the educational institutions such as, schools, colleges (Nursing, Medical, Junior Colleges, College of Yoga and Naturopathy) and girl’s hostels.
Survey instrument
A pre-tested, self-administered questionnaire was used to collect the preliminary data. The questionnaire was intended to obtain information on the age of the subject, age at menarche, socio-economic status (SES), mode of delivery, family h/o diabetes/thyroid disorder/menstrual irregularities, dietary habit, h/o migration after attaining menarche and habit of daily physical exercise. Each question was explained in detail and questions translated in local vernacular language were served to the subjects of non-English medium of education. After the questionnaire was filled, the individuals were subjected to general examination (presence of wisdom tooth/alopecia/hirsutism and anthropometry) and the data were collected using a standard case study form. Study subjects with suspected PCOS underwent an abdominopelvic ultrasound scan and a thyroid profile. All variables were dichotomous except migration, which was coded as 0, 1 and 2 for never migrated, migrated more than twice and migrated once or twice after attaining menarche respectively. More than 1 month stay in a migrated place was considered as migration. Low socio-economic (LSE) status was designated based on the availability of “Arogyasri” card, [9] (A card distributed to the people of below the poverty line to provide free medical and health services in Andhra Pradesh). A waist-hip ratio of more than 0.85 was considered as central obesity.
Diagnosis of PCOS
PCOS was suspected among the study subjects using the Rotterdam’s diagnostic criterion. [10] PCOS was said to be present if two of the three criteria, [1] oligo-ovulation and/or anovulation, [2] hyperandrogenism (clinical or biochemical). In the present study, clinical diagnosis was performed based on the hirsuitism (Ferrimen and Gallwey Scale), acne, androgenic alopecia and virilization, [3] polycystic ovaries (by gynecological ultrasound by specifically looking for the bilateral presence of multiple sub-cortical ovarian cysts arranged in a necklace pattern) were met.
Statistical methods
SPSS 12.0 software (SPSS Inc., Chicago, II, USA) was used for the statistical analysis. Continuous variables were expressed in mean ± standard error of mean (SEM) and categorical variables were expressed as proportions. Pearson’s Chi-square (χ2 ) test was used to evaluate the differences in proportions between the groups. Binary logistic regression analysis was performed with PCOS as dependent variable and other statistically significant variables as independent to elicit the strength of association. A P < 0.05 was considered as statistically significant.
| Results |
The study subjects belonged to a heterogeneous population comprised of 253 adolescent girls, 116 belonging to high socio-economic group and 137 from LSE group. Data was missing in the self-administered questionnaire for the variable mode of delivery in 0.8% of cases and for family h/o menstrual irregularities in 0.4% of cases.
The mean age of the subjects was 18.57 ± 0.19 years (SEM) and the mean age at menarche was 13.28 ± 0.08 years (SEM). The prevalence of PCOS in this subpopulation was 15.4% (95% confidence interval: 10.97-19.83). In univariate analysis as illustrated in [Table 1], PCOS was significantly associated with higher SES, presence of wisdom tooth, delivery by cesarean section, family h/o menstrual irregularity, non-vegetarian diet, central obesity and hypothyroidism. The results of the binary logistic regression analysis by enter method using PCOS as dependent and other statistically significant variables as independent are shown in [Table 2].
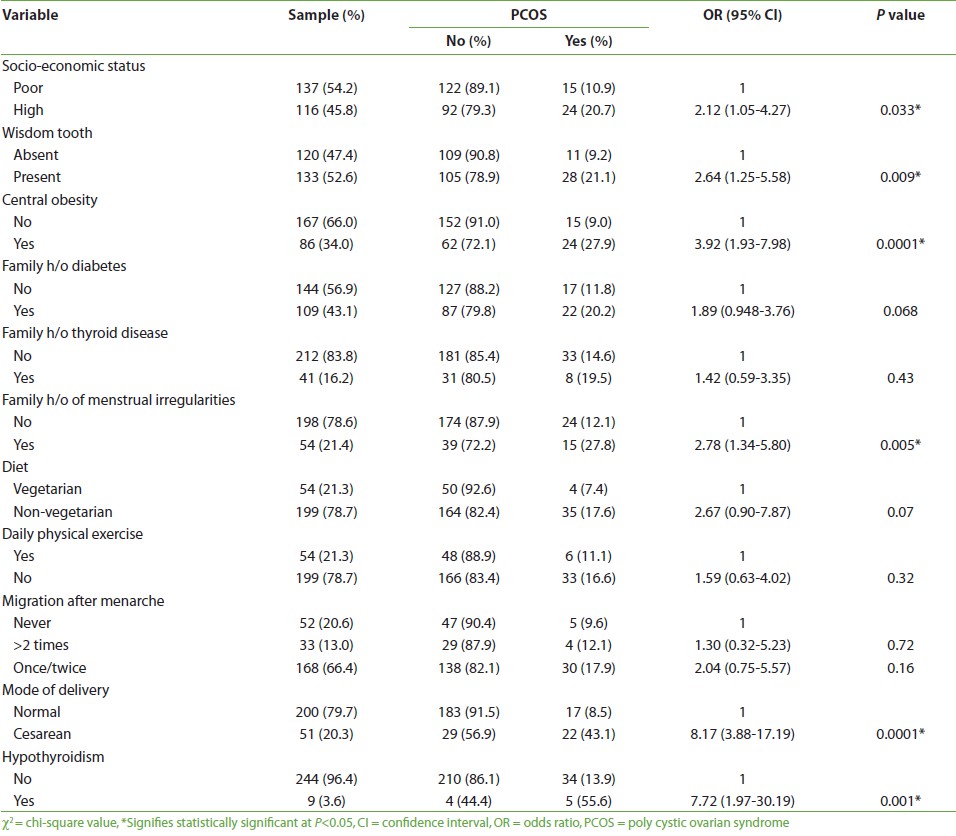 |
Table 1: Univariate analysis of factors associated with PCOS, among adolescent females
Click here to view |
| Table 2: Multi-variable binary regression analysis of factors associated with PCOS*
Click here to view |
| Discussion |
In the present day context, PCOS is a significant health problem in adolescent females mainly because it targets the women during her golden productive age affecting education and work and there by indirectly affects the Nation’s productivity. The prevalence and the factors associated with PCOS were investigated in a community-based questionnaire survey among the adolescent females in Nellore district, Andhra Pradesh. This study showed that an adolescent girl delivered through C-section, having erupted at least one wisdom tooth and with central obesity is significantly at a higher risk of developing PCOS then her counterparts. Though similar associations have not been observed earlier, in the published repository, an attempt has been taken to hypothesize causal relationship from the available literature.
Alterations in the dopamine levels by cesarean mode of delivery was studied in the rat model, [11] which showed that in the rats born through the rapid C-section, post-pubertal dopamine levels were less in the prefrontal cortex and more in the nucleus accumbens. The control group was a set of rats delivered through normal vaginal delivery. Hypothalamus receives numerous projections from the prefrontal cortex. [12] Hence, when dopamine levels decreases in the prefrontal cortex, it decreases in the hypothalamus too. Dopamine usually exerts an inhibitory action over the release of gonadotrophin releasing hormone (GnRH). Hence, decrease in dopamine in the hypothalamus causes an increase in GnRH pulsations [13] that in turn acts on pituitary to increase the luteinizing hormone (LH) levels. Increase in the LH levels (LH dominance) is an important endocrinological event that plays a key role in the pathogenesis of PCOS. [14] Therefore, cesarean mode of delivery produces long-term alterations in the dopaminergic system [15] that affects the hypothalamo-pitutary-ovarian axis, which may lead to PCOS.
Further, PCOS has been found to have a hereditary background. [16] So if a woman suffers from PCOS, there is a likely hood of infertility and the pregnancy becomes a precious one, which eventually goes for C-section. At the same time, PCOS also has a firm background of insulin resistance, [17] which is again inheritable. So if the mother had suffered from gestational diabetes, she may probably go for C-section because of her big baby. Ultimately, the female child, having inherited the abnormality (of PCOS or insulin resistance) and born through C-section, may develop PCOS at a later age. Additional rigorous study designs are intended to delineate the exact pathogenesis.
In all countries, at all ages, males are ahead in development of third molar (wisdom) tooth compared to females. [18] This makes it evident that the male sex hormones may hasten the growth of wisdom tooth. Since, hyperandrogenism is a well-known phenomenon in the PCOS individuals; it probably contributes to the co-existence of development of wisdom tooth and PCOS, though causal relationship is difficult to outline in the present context. In another study, [19] investigators have divided the third molar tooth based on the root development stage (complete and incomplete root development). On immune-staining, they found that the expression of insulin like growth factor-1 and proliferating cell nuclear antigen to be significantly higher in cells of pulps having complete root development, which may again be related to insulin resistance.
Colombo et al. [20] documented the relationship between the dietary surveys of subjects with anovulation (hypothalamic anovulation and PCOS), which showed though the macronutrient intake was similar in both groups, the body mass index and body fat was reported to be more among the PCOS individuals. Similarly, a study on obesity and PCOS demonstrated 28.3% prevalence of poly cystic ovarian disease in overweight and obese women from Spain [21] and yet another study, [5] encountered obesity in 30-70% of PCOS affected women. There is a complex association between PCOS and obesity. LH dominance leads to increased ovarian androgen production, which in turn results in androgen receptor mediated insulin resistance in the adipocytes. [22] Due to which, the insulin mediated inhibition of very low density lipoprotein (VLDL) synthesis is lost [23] and there is raised VLDL synthesis leading to obesity. Obesity further perpetuates the hyperandrogenemic state and the vicious cycle continues. It has been reported that non-vegetarians have an unfavorable lipid profile, [24] with increased low density lipoprotein, VLDL and total cholesterol levels and decreased high density lipoprotein levels. This leads to obesity that predisposes to PCOS through hyperandrogenism and insulin resistance. In our study, we have found an association between the non-vegetarian diet and PCOS in the univariate analysis, which failed to show an association in the final regression model. Larger sample is probably required to refute this hypothesis.
Stress is a well-known factor that leads to alteration in the normal physiological functioning of the body. Many girls complain of missing periods or having irregular cycles when they go through stressful periods. Stress due to migration has also been attributed to affect the hormonal profile of the individual. [8] However; contrary to our preliminary hypothesis of association between migration and PCOS, the final regression model eliminated this variable, though univariate analysis showed migration of once or twice had statistically significant association with PCOS.
| Conclusion |
The prevalence of PCOS in Nellore district is 15.4%. Several factors influencing the occurrence of this syndrome have been investigated earlier. Our study contributes further to the body of evidence for occurrence of PCOS by bringing out many interesting risk factors that open up new approaches toward the prevention and management of polycystic ovarian syndrome. The future work involves establishing biochemical and genetic relationship between the cesarean mode of delivery and the presence of wisdom tooth to the occurrence of PCOS.
| References |
| 1. | Allahbadia GN, Merchant R. Polycystic ovary syndrome in the Indian Subcontinent. Semin Reprod Med 2008;26:22-34. |
| 2. | Haugaard LK, Vestergaard H, Skouby SO. Polycystic ovary syndrome and comorbidity. Ugeskr Laeger 2010;172:199-202. |
| 3. | Deeks AA, Gibson-Helm ME, Teede HJ. Anxiety and depression in polycystic ovary syndrome: A comprehensive investigation. Fertil Steril 2010;93:2421-3. |
| 4. | Jedel E, Waern M, Gustafson D, Landén M, Eriksson E, Holm G, et al. Anxiety and depression symptoms in women with polycystic ovary syndrome compared with controls matched for body mass index. Hum Reprod 2010;25:450-6. |
| 5. | Vrbikova J, Hainer V. Obesity and polycystic ovary syndrome. Obes Facts 2009;2:26-35. |
| 6. | Goldenberg N, Glueck C. Medical therapy in women with polycystic ovarian syndrome before and during pregnancy and lactation. Minerva Ginecol 2008;60:63-75. |
| 7. | Boomsma CM, Fauser BC, Macklon NS. Pregnancy complications in women with polycystic ovary syndrome. Semin Reprod Med 2008;26:72-84. |
| 8. | Falk RT, Fears TR, Hoover RN, Pike MC, Wu AH, Nomura AM, et al. Does place of birth influence endogenous hormone levels in Asian-American women? Br J Cancer 2002;87:54-60. |
| 9. | Webpage. Arogyasri Health Care Trust, Quality Medicare for the Unreached. Available from: https://www.aarogyasri.org/ASRI/index.jsp. [Last accessed on 2011 Nov 24]. |
| 10. | Broekmans FJ, Knauff EA, Valkenburg O, Laven JS, Eijkemans MJ, Fauser BC. PCOS according to the Rotterdam consensus criteria: Change in prevalence among WHO-II anovulation and association with metabolic factors. BJOG 2006;113:1210-7. |
| 11. | El-Khodor BF, Boksa P. Long-term reciprocal changes in dopamine levels in prefrontal cortex versus nucleus accumbens in rats born by caesarean section compared to vaginal birth. Exp Neurol 1997;145:118-29. |
| 12. | Ongür D, An X, Price JL. Prefrontal cortical projections to the hypothalamus in macaque monkeys. J Comp Neurol 1998;401:480-505. |
| 13. | Henderson HL, Townsend J, Tortonese DJ. Direct effects of prolactin and dopamine on the gonadotroph response to GnRH. J Endocrinol 2008;197:343-50. |
| 14. | Blank SK, McCartney CR, Marshall JC. The origins and sequelae of abnormal neuroendocrine function in polycystic ovary syndrome. Hum Reprod Update 2006;12:351-61. |
| 15. | Juárez I, De La Cruz F, Zamudio S, Flores G. Cesarean plus anoxia at birth induces hyperresponsiveness to locomotor activity by dopamine D2 agonist. Synapse 2005;58:236-42. |
| 16. | Zhuo G, Feng G, Leng J, Yu L, Jiang Y. A 9-bp deletion homoplasmy in women with polycystic ovary syndrome revealed by mitochondrial genome-mutation screen. Biochem Genet 2010;48:157-63. |
| 17. | Kent SC, Gnatuk CL, Kunselman AR, Demers LM, Lee PA, Legro RS. Hyperandrogenism and hyperinsulinism in children of women with polycystic ovary syndrome: A controlled study. J Clin Endocrinol Metab 2008;93:1662-9. |
| 18. | Thevissen PW, Fieuws S, Willems G. Human third molars development: Comparison of 9 country specific populations. Forensic Sci Int 2010;201:102-5. |
| 19. | Caviedes-Bucheli J, Canales-Sánchez P, Castrillón-Sarria N, Jovel-Garcia J, Alvarez-Vásquez J, Rivero C, et al. Expression of insulin-like growth factor-1 and proliferating cell nuclear antigen in human pulp cells of teeth with complete and incomplete root development. Int Endod J 2009;42:686-93. |
| 20. | Colombo O, Pinelli G, Comelli M, Marchetti P, Sieri S, Brighenti F, et al. Dietary intakes in infertile women a pilot study. Nutr J 2009;8:53. |
| 21. | Alvarez-Blasco F, Botella-Carretero JI, San Millán JL, Escobar-Morreale HF. Prevalence and characteristics of the polycystic ovary syndrome in overweight and obese women. Arch Intern Med 2006;166:2081-6. |
| 22. | Corbould A. Chronic testosterone treatment induces selective insulin resistance in subcutaneous adipocytes of women. J Endocrinol 2007;192:585-94. |
| 23. | Wetterau JR, Lin MC, Jamil H. Microsomal triglyceride transfer protein. Biochim Biophys Acta 1997;1345:136-50. |
| 24. | Melby CL, Toohey ML, Cebrick J. Blood pressure and blood lipids among vegetarian, semivegetarian, and nonvegetarian African Americans. Am J Clin Nutr 1994;59:103-9. |
Source of Support: STS scholarship for 2 months (Rs. 10, 000/-)., Conflict of Interest: None
| Check |
DOI: 10.4103/1755-6783.140233
| Tables |
[Table 1], [Table 2]



