Objective: The objective of this study was to determine whether white blood cell (WBC) count at admission can predict hemoglobin (Hb) drop in multiple trauma patients and can be considered a predictive sign for the need for transfusion of packed red blood cells in multiple trauma patients. Patients and Methods: This retrospective study was performed on 227 trauma patients, evaluated over a 30-month period (January 2014 to July 2016). Data collected included demographics, injuries, leukocyte count, and Hb at admission time of 0, 24 h, 48 h, transfusion requirement. Leukocytosis and Hb drop were defined as leukocyte count ≥16,000/mm3 and 2 g/dL, respectively. We compared two groups of multiple trauma patients with leukocytosis at admission time and normal WBC count with Hb drop in hospital course. The patients had similar injury severity scores. Data were analyzed by SPSS version 21. Results: Of the 227 patients admitted for durations longer than 24 h, WBC count was available for them. Leukocyte count showed a strong association with severe injury (P = 0.01). The logistic regression was used for the prediction of Hb drop of participant. The Cox and Snell R Square and Nagelkerke R Square indicated that the variances in this research between 0.006 and 0.008 have been explanations. Conclusion: The results showed that early leukocytosis has a relationship with severity of injury, but it is not beneficial in predicting Hb drop and transfusion requirement. Keywords: Hemoglobin, leukocytosis, multiple trauma, transfusion packed cell
Identification of significant injury in the trauma patients remains a difficult task. Having early markers of injury may help the clinician prevent serious decompensation of patients and thereby improve their outcome and hasten their disposition.[1] Emergency physicians are continually seeking early markers that efficiently differentiate trauma patients with major injuries from those with minor injuries.[2] Vital signs with blood pressure and pulse rate cannot predict significant injury in multiple trauma patients. Furthermore, normal vital signs cannot exclude solid organs or visceral or vascular ones. Multiple injuries are considered major stressful conditions, which induce neuronal and hormonal responses, epinephrine and cortisol, producing leukocytosis from both bone marrow and splenic sources.[3],[4],[5] Since complete blood analysis is one of the first tests obtained from trauma patients in the emergency department, white blood cell (WBC) count can serve as an easily obtained marker for a serious injury.[6] Multiple injured patients seem to have elevated – or at least high normal – WBC count values on presentation. This suggests that the stress of trauma incident itself can result in marked demargination.[6] For this reason, patients with multiple trauma would have increases in WBC count. The patients with severe injuries may require transfusion of packed cell on hospital course. For this, we should prepare packed cells and be ready for transfusion. In this article, we hypothesized that increases in WBC could predict hemoglobin (Hb) drop in hospital course.
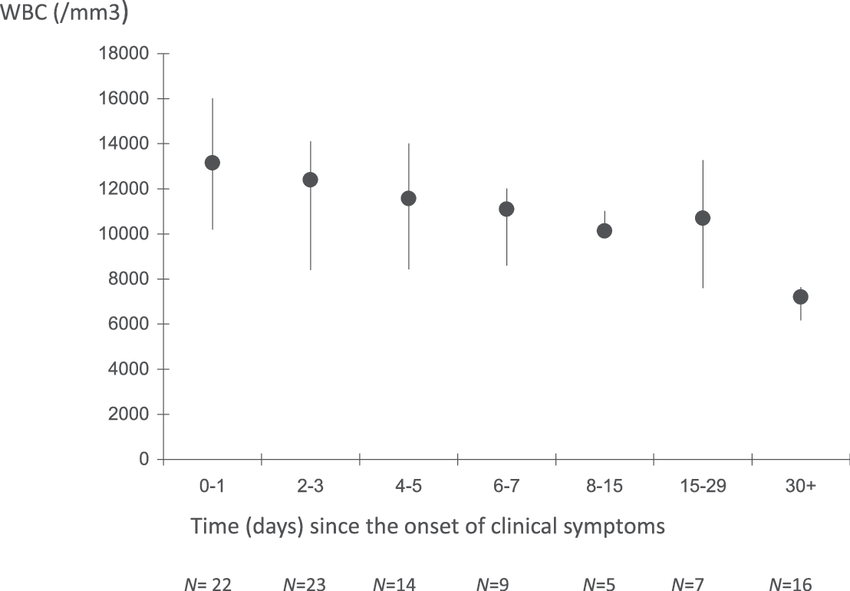
This retrospective study was performed on 227 trauma patients. We measured the WBC count and Hb of patients who came to Peymanieh Hospital Emergency Center over a 30-month period (January 2014 to July 2016). Data collected included demographics, injuries, leukocyte count, and Hb at admission time of 0, 24 h, 48 h, and transfusion requirement. Leukocytosis and Hb drop were defined as leukocyte count ≥16,000/mm 3 and 2 g/dL, respectively. Patients excluded from our study were those with obvious injuries requiring immediate surgery, patients transferred from other institutions, or those dead on arrival. The diagnosis and disposition of these patients are either already determined, as in the case of transfers, or obvious for patients in need of emergent surgery, or who were dead on arrival. Patients who went immediately to the operating room included transabdominal gunshot wounds or blunt or penetrating torso injuries that were hemodynamically unstable.[7] We also excluded all patients with isolated head trauma. We compared two groups of multiple trauma patients. One group comprised the patients who had normal WBC count at complete blood count analysis of admission time: they had moderate-to-severe injury, without isolated head trauma, and/or extremity-isolated trauma, or they had multiple trauma. Data were collected. The other group comprised the patients with leukocytes higher than normal range. These patients also had multiple trauma, without isolated head or extremity trauma. Two groups were admitted to hospital for more than 2 days and Hb followed. In our study, patients who went to the surgery room at the time of admission or those who died before 6 h at the time of admission were excluded from the study. Data collected and groups were compared with each other for the range of Hb drop and required transfusion of packed cell. The logistic regression was used for the prediction of Hb drop of participants. The goodness of fit test (Hosmer and Lemeshow test) with P > 0.05 showed that logistic regression is possible.
In a total of 227 participants, mean ± standard deviation of age was 34.30 ± 18.66 years. Males numbered 182 and 80.17% of all multiple trauma patients. As collected from these patients, 75 persons required surgery. This means 33.3%, and for 144 patients, brain computed tomography scan had been done. The demographic and clinical characteristics of the study population were categorized and reported in [Table 1].
The logistic regression was used to predict the Hb drop of participant. The goodness of fit test (Hosmer and Lemeshow Test) with P > 0.05 showed that logistic regression is possible. The Cox and Snell R Square and Nagelkerke R Square indicated that the variances in this research between 0.006 and 0.008 have been explanations. The WBC count for the normal group was lower than 16,000, and for the group of patients with leukocytosis, it was ≥16,000/mm 3 and more than it. Hb drop was mean ≥2 g/dL. These two groups were compared with each other for Hb drop in the course of hospitalization. The results of calculation B and Exp (B) showed that leukocytosis has no correlation with Hb drop [Table 2].
Finally, the regression equation: ⋆Ratio of yes/no in Hb drop. Hence, leukocytosis is a predictor of the severity of injury in multiple trauma patients but cannot predict that every patient with severity injury and leukocytosis may undergo a Hb drop in future. On the other hand, it is true that hemoconcentration can cause leukocytosis but cannot cause errors in detection of Hb in real. Hb has no association with hemoconcentration and leukocytosis.
The number of patients with severe injury caused by release of catecholamine and demargination WBC count is higher than normal in multiple trauma patients. This article showed that severity of injury was able to increase WBC count but did not have any effect on Hb to keep it in the normal range of pseudonormalization. There is no correlation between the severity of injury, leukocytosis at admission time, and Hb drop in course of hospitalization.
Leukocytosis at admission time cannot predict Hb drop in future, and we cannot decide whether or not to prepare packed cell for patients with leukocytosis. Financial support and sponsorship Nil. Conflicts of interest There are no conflicts of interest.
Source of Support: None, Conflict of Interest: None
[Table 1], [Table 2] |
|||||||||||||||||||||||||||||||||||||||||||||