|
The clinical spectrum of amoebiasis is broad ranging from asymptomatic passage of cysts through fulminant colitis to localized abscesses of the liver, lung, brain, and other tissues. Amoebic liver abscess (ALA) is a serious, but readily treatable form of hepatic infection. It usually presents with high-grade fever, associated with right upper abdominal pain, constitutional symptoms, and pleuropulmonary complications mainly in the form of pleural effusion and leucocytosis. However, pneumonitis, leukemoid reaction, and jaundice are an uncommon association. We hereby report a young nonalcoholic immunocompetent female, diagnosed to have ALA associated with multiple unusual complications,who showed excellent response to intravenous metronidazole.
Keywords: Amoebic liver abscess, leukemoid reaction, pneumonitis
How to cite this article:
Chaudhary SC, Avasthi R, Safal, Mohanty D. Amoebic liver abscess: Unusual manifestations. Ann Trop Med Public Health 2013;6:128-30 |
How to cite this URL:
Chaudhary SC, Avasthi R, Safal, Mohanty D. Amoebic liver abscess: Unusual manifestations. Ann Trop Med Public Health [serial online] 2013 [cited 2017 Nov 14];6:128-30. Available from: https://www.atmph.org/text.asp?2013/6/1/128/115190 |
India is an endemic zone for Entamoeba histolytica infection, and amoebic liver abscess (ALA) is the commonest extraintestinal manifestation of the same. The incidence of ALA has been reported to vary between 3% and 9% of all cases of amoebiasis. The disease has a strong male preponderance,wide clinical spectrum ranging from an asymptomatic, even self-limiting course to an acute infection with myriad complications and high mortality. Here, we discuss a case of right lobe ALA with right lower zone pneumonia, leukemoid reaction, and jaundice, which responded dramatically to treatment with metronidazole.
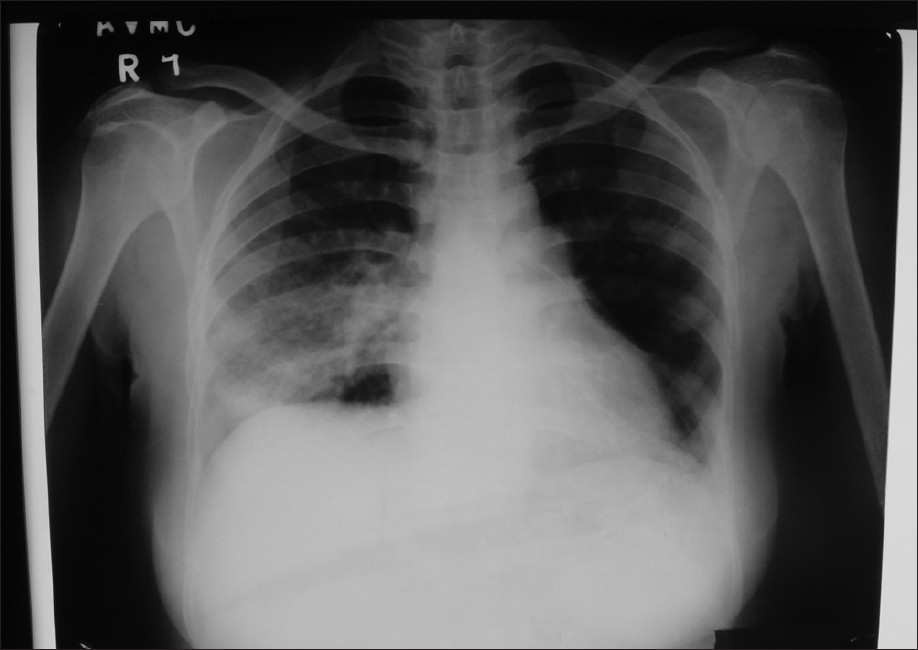
A 26-year-old female was referred from a private hospital on postpartum day 12 with complaints of high grade fever with chills, productive cough, progressively increasing breathlessness, right upper quadrant abdominal pain, and swelling all over body for last 10 days. History of intravenous antibiotics (ceftriaxone × 10 days) and transfusion of two units of blood were present. There was no history of antepartum or postpartum hemorrhage, alcohol intake, jaundice and blood transfusion in the past. On examination, her general condition was poor, she had a blood pressure of 100/70 mmHg, pulse 96/min, respiratory rate 24/min, pallor, raised jugular venous pressure, bilateral basal coarse crepts (R>L), and moderate hepatosplenomegaly. Investigations revealed hemoglobin of 7.5 g%, total leukocyte count 67,500/mm 3 , differential leukocyte count P70L28E1M1, platelet count 38,000/mm 3 , and ESR was 80 mm in 1 st h. Peripheral blood smear showed mild to moderate hypochromia, moderate anisocytosis, neutrophilic leukocytosis with mild shift to left and reduced platelets. Her total serum bilirubin was 3.25 mg/dl, serum alanine aminotransferase 465 U/l, serum aspartate aminotransferase 663 U/l, serum alkaline phosphatase 1602 U/l, total serum protein 5.6 g/dl (albumin 2.9 g/dl), prothrombin time 15 s (control – 12.3), blood urea 83 mg/dl and serum creatinine 1.1 mg/dl. Chest X-ray showed right lower zone consolidation along with elevation of right dome of diaphragm and borderline cardiomegaly [Figure 1]. ECG revealed sinus tachycardia. Ultrasound showed right lobe liver abscess with hepatosplenomegaly, and there was no evidence of any retained product of conception. Aspirate from the abscess was anchovy sauce in appearance and showed few degenerative chronic inflammatory cells in background of necrotic material. Aspirate was negative for gram stain, AFB stain and PCR for Mycobacterium tuberculosis. Blood, urine and stool cultures were sterile. Hepatitis B surface antigen, hepatitis C virus antibody, and enzyme-linked immuneosorbent assay (ELISA) for HIV were negative. Bone marrow aspiration showed a hypercellular marrow with M:E=2.3:1. Erythroid cells showed normoblastic maturation with some erythroid precursors showing early megaloblastic change and mild dyserythropoiesis. No abnormal cells or parasites were seen. Amoebic serology was positive with titer of 1:512. Diagnosis of ALA with multiorgan dysfunction was kept.
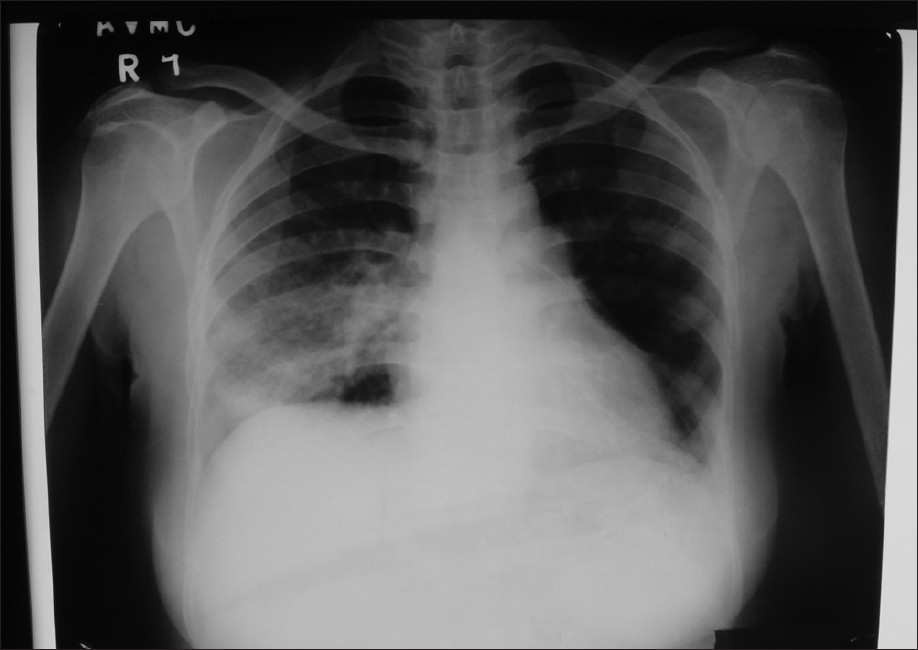 |
Figure 1: Chest radiograph showing haziness in right lower zone along with elevation of right dome of diaphragm and borderline cardiomegaly
Click here to view |
Patient was treated with intravenous metronidazole 500 mg 6 hourly along with supportive management for 14 days to which she showed gradual response and became afebrile on the fifth day of treatment. After completion of metronidazole therapy, she was also given luminal amoebicide (diloxanidefuroate 500 mg thrice a day) for 10 days. Her blood investigations returned to normal after 14 days of treatment. Repeat chest X-ray showed clearing of the consolidation. Ultrasound abdomen showed a thick walled organizing liver abscess [Figure 2]. Contrast enhanced CT scan abdomen and chest showed a large liver abscess in the right lobe of the liver with clear lung fields [Figure 3]. Patient was doing well in her follow-up.
 |
Figure 2: Ultrasound abdomen done after completion of metronidazole therapy showing a large, thick walled organizing liver abscess
Click here to view |
 |
Figure 3: Contrast enhanced CT abdomen and chest showing large right lobe liver abscess
Click here to view |
This patient of ALA is interesting because of diagnostic dilemma at the initial stage and multiple unusual features presenting simultaneously. A differential of ALA with pleuropulmonary complications versus right lower lobe pneumonia with septicemia with pyogenic liver abscess was kept. However, the presence of a single large abscess, a strongly positive amoebic serology, anchovy sauce appearance of the aspirate, sterile serial blood cultures and sterile aspirate culture tilted the diagnosis in favor of ALA. The nonresponse of ceftriaxone given at the primary center for 10 days and the rapid response on addition of IV metronidazole to the same regimen further confirmed the diagnosis. [1]
Hepatic amoebiasis is the commonest extraintestinal manifestation of E. histolytica infection, and it is commonly presented as right upper quadrant pain with fever. Pleuropulmonary complications are among the commonest, though right lower lobe consolidations are less frequent as compared to right pleural effusion. [2] The invasion of lung parenchyma by E. histolytica leads to the development of interstitial pneumonitis followed by liquefaction and formation of lung abscess, which may rupture into a bronchus and provoke vomica, a sudden and profuse expectoration of putrid purulent matter. [3] Splenomegaly, jaundice, and leukemoid reaction are all known to be associated with ALA occasionally. [4] However, a combination of these uncommon findings presenting simultaneously in an immunocompetent nonalcoholic adult female patient is exceedingly rare. An amoebic serology is a useful adjunct in diagnosis with sensitivity approaching 98% for ELISA and 90-100% for indirect haemagglutination test. Demonstration of trophozoites is often not possible in the pus/necrotic material aspirated. The yield is higher if biopsy material is taken from the edge of the abscess, but this may not be advisable in most cases. [3]
After clinical cure, patient shows few symptoms and sonographic follow-up demonstrates evidence of persistent hypoechoic lesion. [5] The mean time for disappearance of the same is 6-9 months. Relapse is very uncommon and sonographic abnormalities do not warrant continued therapy. Factors influencing the healing time and acting as an independent risk factor for mortality include serum bilirubin level >3.5 mg/dl, encephalopathy, larger volume of abscess at admission and hypoalbuminemia (serum albumin <2.0 g/dl). The duration of symptoms and the type of treatment do not influence the mortality. [6]
| 1. |
Hsu MS, Hsieh SM, Chen MY, Hung CC, Chang SC. Association between amebic liver abscess and human immunodeficiency virus infection in Taiwanese subjects. BMC Infect Dis 2008;8:48-52. |
| 2. |
Patney NL, Tandon RK, Srivastava VK. A clinico-pathological study of pleuro-pulmonary amoebiasis and its management. Indian J Tuberc 1974;21:137-44. |
| 3. |
Salles JM, Moraes A, Salles MC. Hepatic amoebiasis. Brazilian J Infect Dis 2003;7:96-110. |
| 4. |
Avasthi R, Agarwal S, Ram BK. Leukemoid reaction in amoebic liver abscess.Indian J Med Sci 1995;49:58-60. |
| 5. |
Reed SL. Amoebiasis and infection with free living amebas. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson L, et al., editors. Harrison’s Principles of Internal Medicine. 17 th ed. New York: McGraw-Hill Medical Publishing Division; 2008. p. 1275-80. |
| 6. |
Sharma MP, Ahuja V. Amoebic liver abscess. JIACM 2003;4:107-11. |
Source of Support: None, Conflict of Interest: None
DOI: 10.4103/1755-6783.115190
[Figure 1], [Figure 2], [Figure 3] |