|
Aspergilloma represents one of the many manifestations of fungus Aspergillus and usually occurs in preexisting lung cavities. It may be asymptomatic or presents sometimes with massive hemoptysis requiring urgent intervention. This patient was not suffering from any predisposing factors for acquiring fungal ball except chronic tobacco use and possible development of COPD. His symptoms and radiological features were suggestive of pulmonary tuberculosis. However as his tuberculin test and sputum were negative, a possibility of fungal ball was kept which was later confirmed by CT scan of chest. The case highlights the role of tobacco in compromising immune status of patient giving way for acquisition of fungal ball in lungs and the role of imaging in early diagnosis of these disorders.
Keywords: Aspergilloma, fungal ball, tuberculosis
How to cite this article:
Aggarwal R, Dwivedi S, Aggarwal M. Aspergilloma. Ann Trop Med Public Health 2013;6:345-6 |
How to cite this URL:
Aggarwal R, Dwivedi S, Aggarwal M. Aspergilloma. Ann Trop Med Public Health [serial online] 2013 [cited 2017 Nov 14];6:345-6. Available from: https://www.atmph.org/text.asp?2013/6/3/345/121004 |
Aspergillus species cause different forms of pulmonary diseases in humans depending on their immune status and pre-existing lung involvement. Aspergilloma [1],[2] is one of these manifestations of Aspergillus and generally occurs in pre-existing lung cavities. Unlike invasive pulmonary aspergillosis, Aspergilloma may not require treatment except when associated with life-threatening hemoptysis. This patient was not suffering from any predisposition factors for acquiring fungal ball except chronic tobacco use and possible development of chronic obstructive pulmonary disease (COPD). His symptoms and radiological features were suggestive of pulmonary tuberculosis. However, as his tuberculin test and sputum were negative, CT scan of the chest was done which confirmed the presence of fungal ball.
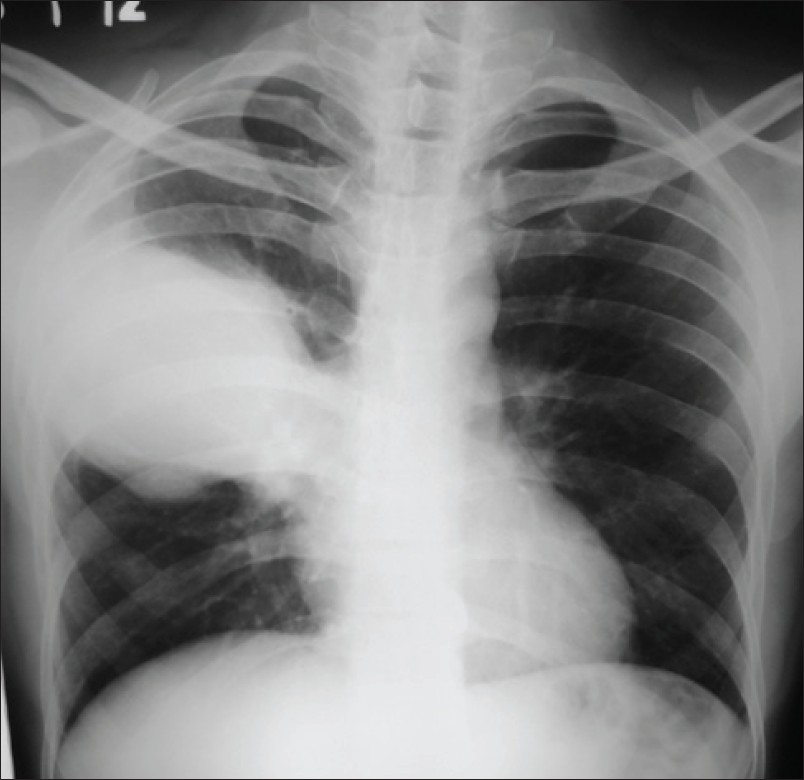
A 37-year-old male came with fever, cough, hemoptysis and chest pain on his right side for last 1 month. He was a chronic smoker and oral tobacco user. He denied any history of tuberculosis or any other chronic illness in the past. On examination his pulse was 100/min, respiratory rate 24/minute and he was afebrile. There was no cyanosis, clubbing or pedal edema. His respiratory system examination was unremarkable except occasional wheezing. HIV was negative and his oxygen saturation was normal. The blood investigations were normal except raised ESR. Pulmonary function tests were suggestive of obstructive airway disease. The chest X-ray revealed a large opacity in the right middle zone [Figure 1]. The closest differential diagnosis initially was made as pneumonia probably of tubercular etiology in view of his prolonged illness and a normal TLC. However, his sputum for AFB and montoux test was negative. A CT scan of the chest was done which revealed a large cavity in the upper lobe with dependent fungal ball in it [Figure 2]. IgG antibodies to Aspergillus were positive in serum. Patient was managed conservatively and started with antifungal drug itraconazole. As he developed massive haemoptysis he had to undergo emergent bronchoscopy for bronchial artery embolization.
|
Figure 2: CT chest: Fungal ball
Click here to view |
Cavities in lung parenchyma have many etiologies like rheumatoid arthritis, sarcoidosis, Wegners granulomatosis, bronchial cysts and bulla, ankylosing spondylitis, neoplasm, pulmonary infarction and tuberculosis. [3],[4] Among these various causes tuberculosis is the commonest cause for causing pulmonary cavities. [5] These residual cavities provide the necessary substrate for colonization by fungus in susceptible individuals. Aspergillus species is spread wide apart in environment and colonization by its species Aspergillus fumigates is mainly responsible for pulmonary diseases. They include invasive manifestations like invasive pulmonary aspergillosis and chronic necrotizing aspergillosis and other noninvasive manifestations like Aspergilloma and allergic bronchopulmonary aspergillosis. Pulmonary aspergilloma usually develops in a pre-existing cavity in the lung and is composed of fungal hyphae, inflammatory cells, fibrin, mucus and tissue debris. Due to lack of adequate drainage from the cavity, the fungus gets an opportunity to grow along the cavity wall. With rare exceptions Aspergilloma generally remains within the cavity and do not invade surrounding parenchyma or blood vessels. [6] This patient was not suffering from any predisposition factors for acquiring fungal ball except chronic tobacco use and possible development of COPD. His symptoms and radiological features were suggestive of pulmonary tuberculosis. However, as his tuberculin test and sputum were negative, CT scan of the chest was done which confirmed the presence of fungal ball.
Tuberculosis may mimic fungal infections radiologically and clinically especially in immunocompetent individuals and therefore use of imaging modalities like CT scan is useful in settling the diagnosis in such cases before treatment regime is planned. Further tobacco use might have been a predisposition for COPD [7] leading to compromised immune status and finally giving way for acquisition of fungal ball in lungs.
| 1. |
Zmeili OS, Soubani AO. Pulmonary aspergillosis: A clinical update. QJM 2007;100:317-34. |
| 2. |
Kousha M, Tadi R, Soubani AO. Pulmonary aspergillosis: A clinical review. Eur Respir Rev 2011;20:156-74. |
| 3. |
Kauffman CA. Quandary about treatment of aspergillomas persists. Lancet 1996;347:1640. |
| 4. |
Zizzo G, Castriota-Scanderbeg A, Zarrelli N, Nardella G, Daly J, Cammisa M. Pulmonary aspergillosis complicating ankylosing spondylitis. Radiol Med 1996;91:817-8. |
| 5. |
Kawamura S, Maesaki S, Tomono K, Tashiro T, Kohno S. Clinical evaluation of 61 patients with pulmonary aspergilloma. Intern Med 2000;39:209-12. |
| 6. |
Rafferty P, Biggs BA, Crompton GK, Grant IW. What happens to patients with pulmonary aspergilloma? Analysis of 23 cases. Thorax 1983;38:579-83. |
| 7. |
Smith NL, Denning DW. Underlying conditions in chronic pulmonary aspergillosis including simple aspergilloma. Eur Respir J 2011;37:865-72. |
Source of Support: None, Conflict of Interest: None
DOI: 10.4103/1755-6783.121004
[Figure 1], [Figure 2] |