Background: Children are one of the most important population groups in the world and malnutrition is considered as one of death causes among them, especially those under 5 years old. The aim of our study was to conduct a systematic review of malnutrition and its associated factors among under five-year-old children of Iran. Materials and Methods: Data were collected through searching electronic databases and searching motors of PubMed, Science Direct, Scopus, Google Scholar, Scientific Information Database, Magiran and IranMedex using key words of “malnutrition,” “under-nutrition,” “stunting,” “underweight,” “wasting,” “factor,” “children,” “under 5 years,” “Iran,” and their Persian synonyms. Some of the relevant journals and websites were hand searched. Results: Of 608 preliminarily retrieved articles, 36 were selected for the final phase of the study. The most important factors related to underweight were mother’s education level, father’s education level, and birth weight. In regard to wasting, gender was one of the main factors and the next four were living location, birth weight, mother’s, and father’s education levels. Mother education level, father education, gender, birth weight, and age group were mentioned as the most important factors resulting in stunting as well. Conclusions: In some regions with low socioeconomic status, especially rural areas, the focus should be on the improvement of households living conditions such as mothers’ and children’s nutrition. Improvement in parents’ education, particularly mothers’ education, can have a significant impact on children’s health. Under 5 years old girls need more attention than boys regarding to their poorer indicators. Keywords: Children, Iran, malnutrition, systematic review, under-nutrition
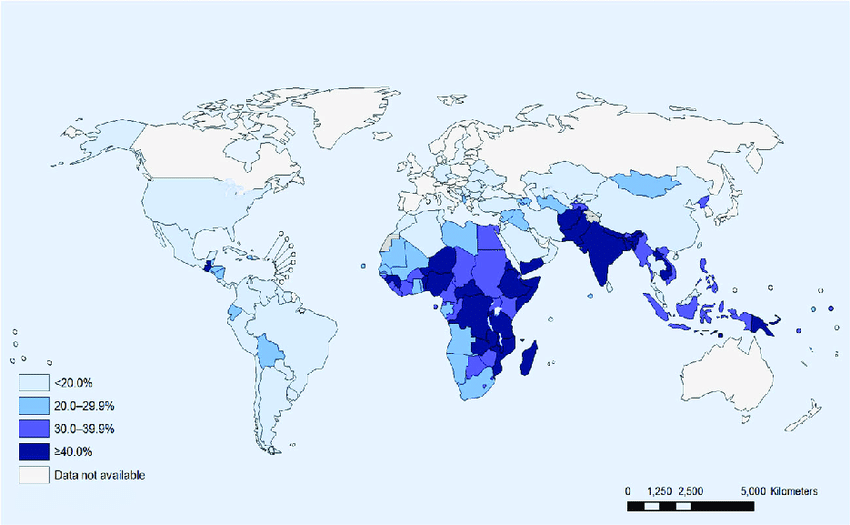
Children are one of the most important population groups in the world and their health is a matter of fundamental importance. In this regard, proper nutrition is a prerequisite for good health. Hence, without ensuring optimal child growth and development, efforts for significant economic development will be unsuccessful.[1],[2],[3] Nutrition has a fundamental role in physical, mental, and emotional development of children, particularly through the formative years of life.[4],[5] The nutritional plans and policies can have important effect on human and social development of communities worldwide.[6] Indeed, malnutrition is considered as one of the most important public health and health policy issues in the world.[7] Malnutrition is a condition causing adverse effects on body form or performance and clinical outcomes due to a deficiency or imbalance of energy, proteins, and other nutrients.[8] Due to their fundamental needs, children are at risk of malnutrition significantly worldwide, especially in developing nations.[9] About 45% of the total mortality is related to under five-year-old children (U5C)[10],[11] among which almost half is attributed to malnutrition.[11] About six million children under age five died in 2015 and the under-five mortality rate in low-income countries was 76 deaths per 1000 live births– about 11 times the average rate in high-income countries (7 deaths/1000 live births).[12] Studies show that despite economic development in developing countries, malnutrition has remained as an important issue.[13],[14] Stunting (low height for age), underweight (low weight for age), and wasting (low weight for height) are key indicators of malnutrition, calculated using anthropometric status of children.[15] In this regard, more than 150 million children suffer from one or more types of malnutrition.[16],[17] The overall prevalence of stunting in the world has been reported 25% which this rate has been 6.6% among Iranian girls. Furthermore, the overall prevalence of wasting among boys in Iran were reported to be 4.11%.[18] Infections and micronutrient and other deficiencies due to inadequate diet are the main causes of malnutrition during childhood.[19] Insufficient food preparation, bad eating habits, psychological factors, family’s food security, and certain metabolic disorders as well as diseases are among factors that limit the intake of food and foodstuff.[5] Besides limited accessing to adequate food and suffering from infections, inadequate access to available hygienic services and issues in the living environment as well as socioeconomic and cultural structure of communities are also considered as primary causes of the incidence and prevalence of malnutrition.[20] In this regard, United Nations International Children’s Emergency Fund (UNICEF) has provided a conceptual model for understanding causes of malnutrition. In this model, main factors are related to socioeconomic, cultural, and political structure of a society.[21] Iran is one of the developing countries and given the importance of this issue in this country, the aim of this study was to conduct a systematic review of factors associated with malnutrition among children under 5 years. The results of this study can identify the most important factors of malnutrition among U5C and lead to improving solutions.
The current systematic review was carried out in June 2016, according to the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) statement.[22],[23] Eligibility criteria The inclusion criteria for the review to identify original studies that investigated factors associated with malnutrition were cross-sectional studies on U5C conducted in Iran without time restrain and language of Persian or English. Case reports, conference presentations, and interventional and qualitative studies were excluded from the study. Data sources Data were collected through searching the electronic databases and searching motors of PubMed, Scopus, Science Direct, Google Scholar, Scientific Information Database, Magiran, and IranMedex using the keywords of “malnutrition,” “under-nutrition,” “stunting,” “underweight,” “wasting,” “wasting syndrome, “factor,” “children,” “under 5 years,” “Iran,” and their Persian synonyms. Some of the relevant journals and websites were hand searched. The reference lists of the selected articles also were checked. Finally, we searched gray literature and contacted experts for possible ongoing studies. Quality assessment Two authors (MM and AA) evaluated the primarily retrieved articles according to the checklist of Strengthening the Reporting of Observational Studies in Epidemiology.[24] The cases in which a consensus was not reached between two reviewers were resolved by consulting a third reviewer (NK). Review process Two leading authors examined each study for the eligibility. Abstracts and if not excluded, the full texts were examined. An extraction form was designed and all relevant information was extracted for analysis. The extraction table included authors, the year study published, the setting of the study, main results, and the final conclusion. For organizing and assessing the titles and abstracts as well as identifying the duplicate entries, a reference management software (Endnote X6) was used. Data analysis Quantitative analysis (meta-analysis) was not done due to existing differences in report of the studies’ results and methodological issues. Descriptive and cross-sectional studies investigating on the factors associated with malnutrition among under five-year-old children were included into the study. Data were summarized into charts by categories (underweight, wasting, and stunting) based on selected factors and the results were reviewed narratively.
Of 608 preliminarily retrieved articles identified through electronic searching, finally 36 articles were included in accordance with the study objectives [Figure 1].
Publication date of studies was between 1997 and 2015. Studies were descriptive-analytical. In 14 studies, the studied age group was related to under 5 years.[25],[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38] There were seven studies on children aged 0–24 months,[39],[40],[41],[42],[43],[44] three on those aged 2–5 years,[45],[46] two studies on children aged under 1 years,[47],[48] and two studies on children aged 1–5 years.[49],[50] Furthermore, there was one study on each of age groups of 0–36 months,[51] 6–24 months,[52] 12–24 months,[53] 6–59 months,[54] 24–35 months,[55] 0–59 months,[56] 25–36 months,[26] and 1–3 years.[57] Two studies were conducted nationwide while other studies were carried out at province or city levels.[31],[32] Furthermore, the most frequently used criterion in the studies to compare with standards was WHO’s growth chart standard (in 26 studies). Extracted information of the reviewed articles are presented in [Table 1].
As [Figure 2] shows, 24 factors affecting underweight among U5C were mentioned totally in the studies. The most frequently mentioned factor was mother’s education level followed by father’s education level and the birth weight. Gender, age group, and birth spacing were the next mentioned factors and 13 remaining factors were mentioned with same frequency in the studied articles.
Twenty-one factors associated with wasting among U5C as shown in [Figure 3]. The most mentioned factor was gender (being girl) followed by four factors including living place (urban or rural), weight birth, mother’s education level, and then father’s education level.
As [Figure 4] shows, 19 factors were related to stunting among U5C. The most mentioned factor was mother’s education level followed by father’s education level.
Gender was found as a meaningful variable associated with malnutrition, i.e., girls were more vulnerable than boys [Figure 6]. Indeed, the number of studies indicated girls’ malnutrition was much more than those showed malnutrition among boys. Furthermore, given the all studies mentioning gender, it can be said that in total and in total average, 74% of the studies mentioned female gender as a factor significantly associated with malnutrition, while 26% pointed to male gender as a factor significantly associated with malnutrition.
Our review showed that gender, mother’s education level, and birth weight are of the most important factors significantly associated with malnutrition among U5C. The wide range of national, social, and economic factors (sometimes so-called “secondary data sets”) contribute to the explanation and understanding of malnutrition among children and also provide a more advanced framework upon which to adopt effective long-term interventions.[60] Studies conducted over the world have indicated that many factors can affect children nutrition. Such factors include socioeconomic status, child or family characteristics, prevalent infectious disease,[14],[61],[62] mothers educational level, limited access to safe drinking water, and poor hygiene,[63] low household wealth index, exposure to open wastewater near the home environment,[64] inadequate purchasing power and access issues, low health literacy and misconceptions regarding proper nutrition and malnutrition, insufficient variety of crops produced.[6] Our review showed that parents’ education level, in particular mothers’, plays a highly important role in their own and children’s health. Many studies considered the role of mothers’ education level and/or their information about children’s nutrition as an effective factor in reducing malnutrition.[6],[30],[34],[36],[46],[50],[63],[59],[58] The role of mothers’ awareness and knowledge regarding issues related to their health and nutrition before, during, and after pregnancy are of great importance. Indeed mothers’ health status can define children’s health both during embryonic and after that. Furthermore, mothers’ awareness and knowledge regarding the fetal health and proper nutrition for child, especially in the first 6 months after birth, can have a vital role in reducing the risk of malnutrition in children.[54] Indeed, the difference in malnutrition among children having higher educated parents is resulted from two factors including higher awareness and higher income in these families. Income is also, in turn, one of the most important factors of access to health care, cultural, and nutritional facilities that can affect nutrition.[65] Birth weight was another important factor mentioned as a factor affecting malnutrition among children under 5 years in the studied articles in our review [Figure 5]. Birth weight is more influenced by status and conditions of mother as well as the status of fetus during embryonic. We also concluded that there were meaningful relationships between gender and nutrition indicators, i.e., girls suffered from malnutrition more than boys in Iran, based on the frequency of reports. The difference between the groups was greater in stunting. According to the UNICEF annual report 2014, the prevalence of wasting in the world have been 8%.[66] The global statistics of 2014 shows that almost one out of 13 children suffers from wasting and one-third of all children suffer from severe wasting.[67] Again more studies reported stunting in girls than boys. Continuous deprivation of adequate nutrition resulting from poverty, frequent infections due to unhealthy environmental situation as well as lack of access to desired care services are the most important causes of nutritional stunting.[68] Stunting represents a long-term malnutrition or illness in children.[15] Thus, long-term assessment and investigation of trends for the evaluation of programs are required. Parents’ educational level, in particular mothers’ educational level, can be mentioned as factors contributing in stunting.
Health policies and programs should focus on factors that cause malnutrition among Iranian U5C. In some regions with low socioeconomic status, especially rural areas, the focus should be on the improvement of households living conditions such as mother and child nutrition. Moreover, the improvement in parents’ education, particularly mothers,’ can have a significant impact on child health. More attention should be taken to promote nutrition equity between girls and boys in Iran. We recommend further studies on the roots of malnutrition among children, especially on factors causing different malnutrition patterns between boys and girls. Acknowledgment This study was part of a PhD thesis supported by Iran University of Medical Sciences (grant No: IUMS/SHMIS _1394/9221557201). Financial support and sponsorship Nil. Conflicts of interest There are no conflicts of interest.
Source of Support: None, Conflict of Interest: None
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6]
[Table 1] |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||